The Human Behind the “Monster.” On the Misrepresentations of Forensic Psychiatry
Dr. Gwen Adshead on How We (Mis)treat Mental Illness
Over the centuries, humans have often turned to the current technologies for metaphors about the mind, and I guess the most common one we hear these days is that of the mind as a computer: a machine where identity is “hard-wired.” Data about thoughts or emotions are “processed” and “filed”; we “switch modes” when carrying out different functions. Such a model of the mind lends itself to some kinds of research but has little to say about the complexity of human experience, especially in the relational space in which we all live our lives. Physicists like Carlo Rovelli tell us that the universe is relational, therefore so the mind must be, and if that is the case, then we need better metaphors, ones that reflect the organic, ever-evolving nature of psychological experience.
I prefer to think of the mind as a coral reef: ancient, layered and mysterious, not without shadows and risk but containing a nourishing diversity; it might appear chaotic, but it is a complex and structured ecosystem, endlessly fascinating and essential to human life. Under environmental stress, many reefs will bleach out and wither, but science has also shown they can be responsive to intervention and made more resilient. As a student, I soon learned that the study of psychiatry would require a “deep dive” below the surface, into a darkness where things of great beauty as well as danger might appear. It would take time to acclimatize myself and learn to breathe easy.
Since then, a long professional voyage has continually inspired in me the awe and wonder that I associate with the ocean and its hidden depths—I love that e. e. cummings idea that it is “always ourselves that we find in the sea.” It has been immensely rewarding work, and often unpredictable; it has shown me how good and evil, ideas of right and wrong, as well as identities like victim and perpetrator, are not set in stone and can coexist. When I started out, I thought the work I was doing was about making people feel better, but time has taught me that it was about helping them to better “know their minds,” which is quite another matter. The process is not painless for my patients, and there has been turbulence for me too along the way. I have found that it is inevitable that I will experience some distressing feelings, though they tend towards deep sadness and frustration more than horror or disgust. It is my job to recognize those responses and hold them with a kind of compassionate detachment, what Buddhists might describe as “hovering in the Bardo.”
As my psychiatric training went on, I found out about forensic work, which looks at the mind’s darker modes that sometimes give rise to risk. The word “forensic” derives from the Latin forum, a place to hear legal disputes. Beyond providing assessment, making diagnoses and coordinating the care of patients like any other medical specialist, forensic psychiatrists address how a society responds to and treats those people who break the criminal law. The work raises fascinating ethical and legal questions about responsibility, agency and blame for actions done when people are mentally unwell. Many forensic psychiatrists work in secure hospitals as members of a team of professionals providing coordinated care; they are like “dive buddies” who discuss a plan and share responsibility for each other’s safety. I am by nature a collaborator, as demonstrated by my work as a group therapist (and, indeed, by the writing of this book), so forensic work seemed an ideal choice for me.
Once I qualified in forensic psychiatry, I soon realized that I wanted to train as a psychotherapist as well. In the early years of the profession, most psychiatrists were also therapists, but by the late 20th century these were seen as separate disciplines and it was considered unusual for a psychiatrist to also offer psychological therapy. Like other medical specialists, they would generally act as case managers, with an overview on assessment and treatment. But, for me, the art of psychiatry was in the dialogue and the story of people’s lives: I wanted to work “in depth” with them and provide time and space for reflection.
In the course of my further training to become a therapist I got involved in particular areas of research such as maternal violence, trauma and group work, as well as medical ethics and the treatment of doctors. These and much more are woven into the tapestry of the lives that follow. An important thread throughout has been my study of childhood attachments in relationships and their association with later violence. This had a major influence on my thinking about human behavior, as I will show.
Every violent crime is a tragedy, for the victims and their families as well as for the perpetrators. I am not here to argue that any violent action should be excused, or that our prisons and secure hospitals should be emptied. I firmly believe in justice and consequences within a humane legal framework and, given some of the terrible things I have seen and heard, I have no doubt that a subgroup of violent offenders belong in secure settings. I also comprehend why some people feel a need to condemn the perpetrators of violence: revenge is a basic human impulse, a kind of wild justice that keeps us stuck in our fear and anger, mirroring the very cruelty we claim to abhor. This can be painful; there is wisdom in that popular notion that hating someone else is like taking poison and waiting for them to die. And, as Gandhi and others have observed, it is a measure of a just society that we treat the worst of us with compassion.
Over the years, I’ve come to think of my patients as survivors of a disaster, where they are the disaster and my colleagues and I are the first responders. I meet them at a turning point in their lives and help them to come to terms with a new identity, which may feel indelible; as one of my patients memorably put it, “You can be an ex-bus driver but not an ex-murderer.” The work we do requires people to take responsibility for their life story, which can be a difficult and lengthy process. This is done in the context of shifting political agendas which shape mental health resources and outcomes.
I well remember how, not long after I started out in my forensic career in the early 1990s, our then prime minister in the UK, John Major, famously said, “Society needs to condemn a little more and understand a little less.” Mandatory minimum sentences and the wave of mass incarceration that followed, coupled with drastic cuts to mental health care services, have had far-reaching and dire social consequences both in the UK and around the world. Much has been written and said about this elsewhere by people far more expert than I; I will just say that we imprison far too many people, essentially to feed the public appetite for punishment, when only a small percentage of them are too cruel or risky to rehabilitate in the community.
I have spent my working life, over 30 years to date, employed within the UK’s National Health Service (the NHS). For much of that time, I’ve been based at Broadmoor Hospital in Berkshire, about 50 miles west of London. Broadmoor was built in 1863 as part of a Victorian system of “asylums” (from the Greek, meaning “refuge”), which were envisaged as places where “criminal lunatics” could be cared for, sometimes indefinitely. With its mock-Gothic appearance and a history of housing some of the UK’s most notorious violent criminals, Broadmoor has long held a particularly lurid place in the British imagination. On a training visit there back in my student days, with all the certitude and ignorance of youth I too thought it was an antiquated and even a barbaric place. When I actually came to work there, I quickly found otherwise. Our secure hospitals fulfill such an important and humane function, and I’m glad to say that most other developed countries have similar psychiatric facilities that either admit people from prison or offer an appropriate alternative for those who need it.
Over the years, I’ve come to think of my patients as survivors of a disaster, where they are the disaster and my colleagues and I are the first responders.
Today, places like Broadmoor are no longer seen as oubliettes for people who cannot be helped and will never be released; on the contrary, the emphasis is on rehabilitation and recovery, with an average stay of five years. At Broadmoor there are around 200 patient beds now, less than half the number there was when I first joined. Many more people are now sent to medium- and low-secure hospitals, where I’ve also worked over the years. Most of the patients in any of these institutions are either committed by a judge after trial, or transferred from prison for treatment if their mental health deteriorates, or (rarely) transferred from community psychiatric outpatient care because of the risk they pose to others.
As some of the following chapters describe, I’ve also spent time working with people inside prisons as an NHS employee. Our mental health services in the UK are mandated to work in prison with inmates with psychiatric problems, and have been since the 1990s. “Inreach teams” do their best to support and treat the unprecedented and ever-growing number of prisoners, and I have seen at first hand how demand for mental health care in prisons far exceeds capacity, and how incarceration exacerbates mental illness; this is a recognized crisis that needs urgent attention.
70 percent of people in UK prisons today are estimated to have at least two mental health issues, ranging from depression to substance misuse and addiction or psychosis. The law-and-order policies introduced in recent years have contributed to sharp increases in the overall prison population, doubling in the UK since I started training as a doctor, while in the US it has more than tripled. Although crime rates in general have fallen in that period, the steep rise in imprisonment rates over time (which is higher in England and Wales than anywhere in western Europe) means that the relative number of people with mental health issues who are incarcerated has also risen.
These numbers are a reflection of serious problems of social and racial inequity in our world, coupled with increasingly punitive approaches to offenders, rather than any causal link between mental illness and crime. The vast majority of people with mental illness will never break any laws at all, not so much as getting a parking ticket, and sadly they are far more likely to be victims of crime. The small cohort of people with an existing mental illness who do end up in prison after committing acts of violence do not do well there; conditions are difficult enough for someone of sound mind and body. The lack of resources means that only 10–20 percent of prisoners will get the help and treatment they need, if they are judged to be “grossly mentally ill.” Even then, they may wait a long time for it; “triage” for the mind is not as straightforward as it is with broken limbs or gunshot wounds.
My therapist colleagues and I have to live with the moral ambiguity and complexity of knowing how flawed and compromised the system is. We are part of a democracy, where the people vote for governments and our laws reflect the will of the majority; that means offenders are being treated this way on our behalf. Every time I work with one person in difficulties, there are many more just like them that I will never reach. Knowing this doesn’t mean I can throw my hands up in protest and walk away; all doctors go towards suffering and make what difference they can. There are also many people who refuse our help even when it is offered; psychological therapy cannot be forced on anyone.
Little has been written about the field of forensic psychiatry for the public; usually, mental illness and the treatment of violence are mythologized and misrepresented, often in fictional form or in “true crime” depictions which tend to ignore our common humanity. Recently I started to feel a sense of urgency about coming forward at what seems to be a moment of reckoning in the world on so many fronts. The intense debates raging around us daily via rapid communication technologies and in siloed media, about a number of pressing social issues, all seem to me to be shot through with fear. And what is more fearsome than a “monster” who commits a violent crime?
__________________________________
Excerpted from The Devil You Know: Stories of Human Cruelty and Compassion by Gwen Adshead and Eileen Horne. Excerpted with the permission of Scribner, a Division of Simon & Schuster, Inc. Copyright © 2021 by Gwen Adshead and Eileen Horne.
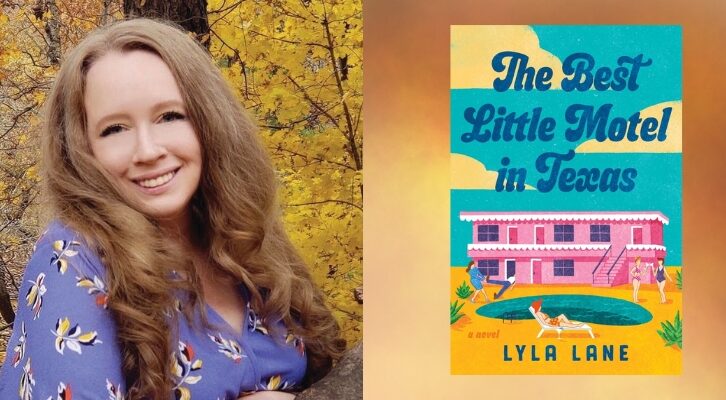
Dr. Gwen Adshead and Eileen Horne
Dr. Gwen Adshead is one of the UK’s leading forensic psychiatrists and psychotherapists. She has spent thirty years working in Broadmoor, England’s largest secure psychiatric hospital, with groups and individual patients convicted of serious violent offenses, as well as with people in prisons and in the community. Gwen has a Masters Degree in Medical Law and Ethics and has published several academic books and over one hundred papers and commissioned articles on forensic psychotherapy, moral reasoning and ethics, and attachment theory. She is a founder member of the International Association for Forensic Psychotherapy and has been a visiting professor at Yale University and Gresham College in the UK.
Eileen Horne is an American author and dramatist currently based in California, with an MA in Creative Writing from the University of London. Following a long career in the UK as an independent TV drama producer, over the last decade, she has written an eclectic mix of historical nonfiction, journalism, Italian translation, as well as several original dramas and literary adaptations—including contributing to a BBC radio drama series about an entirely fictional female forensic psychiatrist.