The Deadly Consequences of Jumping to Conclusions
On the Science of (Un)Fairness in the Criminal Justice System
Jerry Pritchett had stepped out in the cold January night. It was Friday, a little past nine, and Jerry was wearing his slippers. He was just fetching something from his car. But he paused.
There, between the bare ginkgo trees, was a pale, gray-haired man flat on his back in the dim light of a street lamp. The sidewalk that lined the neat brick houses on the north side of Gramercy was empty, save for the body. As Jerry approached, it was clear that something was wrong, but the man couldn’t speak. When Jerry asked him a question, he only groaned in reply. He wasn’t carrying a wallet, but Jerry saw a wedding ring and a watch.
Jerry’s wife, Claude, made the 911 call and then joined her husband. She noticed that the man seemed disconnected: his eyes wouldn’t meet hers, and when she spoke he didn’t seem to understand. He was trying to move himself into a sitting position, but because he was using only the left side of his body, his strength kept giving out, causing his head to pitch back against the concrete. Jerry placed one of his slippered feet under the man’s skull.
Less than ten minutes after the emergency call, four D.C. firefighters pulled up to the house. Almost as soon as they started to attend to the man, he began to vomit.
Claude thought that the man had suffered a stroke, but the firefighters smelled booze. This wasn’t a stroke or heart attack: as one of the firefighters remarked, “Nine out of ten times it’s alcohol-related.” The engine driver found a little blood on the man’s head above the right ear, but there wasn’t any noticeable swelling, and a little pressure applied with a gauze pad stopped the bleeding. They decided not to perform a complete assessment or record the man’s heartbeat, breathing, or blood pressure.
When one of the responding police officers arrived on the scene and asked the firefighters what was wrong, they said that the man was “possibly intoxicated,” that he “fell and hit his head.” As a result, the cops kept to the periphery. According to protocol, they should have worked to secure the scene and begun a preliminary investigation to figure out whether a crime had occurred, but here it didn’t seem necessary: this was just a drunk.
The ambulance carrying emergency medical technicians finally arrived, twenty-three minutes after it was dispatched. “What we got?” the crew leader asked, and one of the firefighters replied, “ETOH,” which is short for ethyl alcohol, the alcohol in wine, vodka, and other spirits. She wasn’t pleased: “We came all this way for an ETOH?”
The firefighters had noticed a few things that didn’t quite add up—the constriction of the man’s pupils, for instance—but they didn’t pass that information along. And neither of the EMTs asked; the man’s condition was as obvious as the foul stench of vomit on his coat. Consequently, they loaded him onto a stretcher without a backboard or neck collar. Given her advanced training, the crew leader was supposed to take charge of the patient, but she got in front to drive without examining the man.
As the assistant EMT did a neurological assessment in the back, he found that the man was barely conscious—scoring a 6 on the 15-point Glasgow Coma Scale, which called for a Priority 1 designation. The assistant, though, classified him as a Priority 3, meaning that he was stable. The man’s inability to form words, his diminished eye and motor responses, just came down to intoxication—nothing to worry about. The assistant skipped the other cognitive tests and left the run sheet blank.
Although Fire and Emergency Medical Services policy requires transporting patients with altered mental status to the closest appropriate facility, the EMTs decided to take the man to Howard University Hospital. It was twice as far away as Sibley, but the crew leader needed to run some personal errands, and Howard was more convenient. The patient could sleep it off in the ambulance just as well as he could at the hospital.
When they arrived at Howard, the EMTs moved the man onto a gurney and told the triage nurse that he was drunk. He was pushed into the hallway and left there; fifteen minutes passed, then thirty, then an hour. The hospital staff didn’t know about the low Glasgow Coma Scale score or any other details about the man, and they, too, took the diagnosis of intoxication at face value. As the triage nurse later explained, she assumed he’d been talking to the EMTs and was now sleeping, so she “just let him sleep.”
No one at the hospital performed the required intake assessments, and when the triage nurse discovered that the man had an abnormally low temperature, she disregarded the information and moved on. After all, it was a cold night. She didn’t check his pupils because that would wake him up, and sometimes when drunks woke up, they became belligerent and tried to leave the hospital. Shining a light in his eyes would just mean taxing an already short-staffed hospital. “I saw he was not in distress so I did not wake him,” she later explained.
When she passed the man off to the charge nurse, the triage nurse said, “We have another ETOH.” And when the team leader for the C and D corridors of the ER was told the same thing, she just “left it alone.” He was not having respiratory problems, so he “was not a priority at that time.” With no reason to rush, the doctor elected to wait for the man’s vomit to be cleaned up before she examined him.
Then something happened that changed everything.
At around 11:30 p.m., another nurse came by to help the team leader sanitize the patient in hallway D. As they were moving the gurney, she noticed that the man’s breathing was different: he now seemed to have a growling snore. That was sometimes a bad sign, so they gave him a sternum rub to check his responsiveness, and the patient “flipped his arms and legs inward.” They repeated the rub, and he reacted the same way.
The nurses couldn’t believe it: he was “posturing,” a common indication of a head injury. But wasn’t this an ETOH? No one had said anything about a head injury.
The doctor saw the posturing from the nurses’ station, and they immediately moved the man to the resuscitation room and called the trauma team.
What had seemed, a moment earlier, to be a routine case of over-imbibing had suddenly become a life-or-death emergency. They intubated the man and now began to discover more cause for concern. His pupils were unequal and did not react normally to light; his breathing was shallow; and they found a small bump and some blood on the side of his head.
They had been looking at things all wrong. The symptoms he exhibited were caused by a neurological injury, not intoxication. And they had wasted hours.
The man was taken in for surgery at 5:50 a.m., more than eight hours after he was first evaluated by emergency medical personnel. It would be for naught.
David Rosenbaum, the award-winning New York Times journalist, died the next day of a brain injury when a blood clot caused his brain to swell. The sixty-three-year-old had retired a month earlier after nearly four decades at the paper’s Washington bureau covering the Capitol’s defining political battles. He had a wife, Virginia; two children, Dorothy and Daniel; and two granddaughters. He lived right around the block from Jerry and Claude Pritchett, on Harrison Street.
How had David injured his head?
The major breaks in the case came down to luck. The lead officer on the scene Friday night when David was put into the ambulance just happened to stay on after his regular shift and answer a radio call about a missing person. When he visited the home and looked at a photograph of the husband who hadn’t returned from his evening stroll, it clicked: this was the same “man down” from earlier in the night on Gramercy Street.
However, it wasn’t until well into Saturday, when credit-card companies called about several suspicious purchases on David’s accounts, that the police realized the extent of their mistake. This was a possible robbery and assault, and they hadn’t even secured the crime scene. The perpetrator or perpetrators had been given almost an entire day’s head start.
But they caught a break. After seeing coverage of David’s death on the news, Michael Hamlin, a twenty-three-year-old maintenance worker, walked into the Seventh District police station to tell his story. Hamlin later claimed that it was out of remorse—the incident was “bearing on his conscience”—though there was some evidence that he thought he might be able to talk his way out, or at least avoid deeper trouble.
According to Hamlin, he had picked up his cousin, Percy Jordan Jr., that night in his green Cadillac. He noticed the hard plastic pipe that Jordan, forty-two, had in his backpack and asked what it was for, to which Jordan shot back, “You know what it’s for.” As they drove, Jordan said, “Let’s go get someone,” adding that they should “go into some of the nice houses they got up there,” by which he meant David Rosenbaum’s northwest D.C. neighborhood. After they parked, they spotted a man with headphones walking down the street, and Jordan went to hide behind a tree right in front of the Pritchetts’ house. When David passed by, Jordan grabbed him, hit him in the head and waist with the pipe, and said, “Give it up, old man.” The force of the blows cracked two of David’s ribs and fractured his skull. With David on the ground, Hamlin ran over and grabbed the wallet out of his back pocket.
It was a good score: around $270 in cash, which Jordan and Hamlin split, along with various credit and debit cards. Leaving the area, they used one of the cards to fill up the gas tank and purchase some snacks. They were back in the car, eating chips and sipping juice, before David was even discovered by the Pritchetts.
* * * *
Lady Justice wears a blindfold. Visit the Supreme Federal Court of Brazil in Brasilia or the Shelby County Courthouse in Memphis, Tennessee, and you will see her: sword in one hand, balance in the other. As the great champion of liberty William Penn once explained, “Justice is justly represented blind, because she sees no difference in the parties concerned. She has but one scale and weight, for rich and poor, great and small.” That is as true for victims as it is for suspects and defendants. The identity of the victim does not influence police work, prosecutions, or sentences. Every man or woman is the same in the eyes of the law.
At least, that’s what we’re told. When seventeen-year-old Trayvon Martin, an African American, was shot and killed by George Zimmerman, a neighborhood watch leader, in a gated community just outside Orlando, Florida, many around the country expressed outrage that Zimmerman had not been arrested immediately. It seemed to be a clear case of racial bias: when young black men are killed, no one cares. But the special prosecutor, Angela Corey, pushed back: “We only know one category as prosecutors, and that’s a ‘V.’ It’s not a ‘B,’ it’s not a ‘W,’ it’s not an ‘H.’ It’s ‘V,’ for victim. That’s who we work tirelessly for. And that’s all we know, is justice for our victims.” Ask any D.A., any police captain, any judge, and that’s the official line.
But how accurate is this narrative of equal justice?
Consider the case at hand. It can be divided neatly into two distinct periods: the time when the victim was John and the time when he was David. When his nametag read John Doe ETOH, firefighters, EMTs, nurses, and doctors neglected rules and procedures, ignored responsibilities, and went through the motions. The police, for their part, did not interview potential witnesses, try to identify the victim, canvass the neighborhood, collect any evidence, or question why an apparently intoxicated person had no wallet. The headphones that were found next to John’s body in the grass were simply left at the scene. When the lead officer was asked whether he had filled out the mandatory incident report, he replied, “No, not for a drunk.”
Once “the drunk” was identified as David Rosenbaum, however, things swung in the opposite direction. There were suddenly newspaper stories and official investigations of the emergency response. When the media and the police realized that the victim on Gramercy Street had been a reporter and editor at the most prestigious paper in the United States, when more than seven hundred people showed up at the memorial service—including Arlen Specter, Orrin Hatch, and Ted Kennedy—and when David Pryor, the former Arkansas senator, remarked that “the echo of [David’s] footsteps and the pounding of his noble heart will be heard for generations to come,” it became, quite simply, a different case.
Indeed, with David in the role of the victim, the D.C. government was prompted to consider sweeping changes to emergency and police procedures. And prosecutors, now under great pressure to serve up justice, convinced Hamlin to plead guilty to the lesser charge of second-degree murder, in exchange for testifying against Jordan. Hamlin was sentenced to twenty-six years; Jordan received sixty-five after a first-degree conviction.
If Lady Justice swung her sword for David, why did she sit idly by for John as he moaned for help? The problem is not, as the playwright David Mamet once glibly suggested, that justice is also deaf; it’s that even as she genuinely believes in her blindness, her eyes are actually taking in quite a lot of information. And once she has a picture of you in her head, that picture has a profound impact on how she goes about her job.
Recent research in psychology sheds light on this process and helps explain the central mystery of David’s case: how so many different professionals—police officers, firefighters, nurses, doctors, and EMTs—specifically charged with helping people and saving lives, made so many errors, from the second David was found lying on the ground to the moment he was transferred to the trauma team at the hospital. It isn’t a story of a few weak links. In the words of the D.C. inspector general’s sixty-nine-page report, prepared in the wake of the incident, there was “an unacceptable chain of failure.” What propelled responders to forgo established protocols, overlook obvious concerns, cut corners, and disregard evidence? The answer lies in how we assess a victim in the wake of a crime. The common assumption is that we gather information through our senses and then, after careful evaluation, reason our way to a complete picture of the person. We use that picture where it is relevant (for example, in coming up with a profile of a serial killer) and put it aside when it is not (determining how much effort to dedicate to securing the crime scene).
In fact, we are not such cool and deliberate detectives; rather, we are masters at jumping to conclusions based on an extremely limited amount of evidence. The automatic processes in our brain (commonly referred to as System 1) quickly take in the scene and then reach a conclusion about the victim based on what is right in front of us, without considering what we might be missing. Ambiguity and doubt are pushed to the side.
In certain circumstances, our more deliberative and effortful mental processes (System 2) can override those initial impressions—and raise the specter of uncertainty—but often, they do not. The less we know, the easier it is for us to produce a coherent story, and it is the consistency of the narrative that predicts how much confidence we will have in our assessment. The unfortunate result is that we may become overconfident precisely when we have limited or weak evidence.
Consider the following two sentences:
When an elderly woman gets on the train, Carl immediately gives up his seat.
When an elderly woman gets on the train, Alex remains in his seat, reading his book.
Which man is likely to come to the aid of a passenger having a heart attack? Easy, right? It is obviously Carl.
But now look back at the sentences. They tell us almost nothing that would help us accurately forecast each man’s future actions. Carl might not have seen the woman at all; he might have given up his seat after suddenly realizing it was his stop, or to move away from a crying child. And Alex might have remained seated because there were many open seats on the train, or because someone else offered the woman a seat and she refused, or because his back was turned. We took a few bits of information and then quickly filled in what was missing, so that we had a coherent story that allowed us to divine the men’s characters and predict how they would behave. We do this hundreds of times a day.
Before you finished reading about the events on Gramercy Street, your mind, too, was busy filling in the details, elaborating scenes and conversations, sizing up the characters, and solving the case. We all fancy ourselves expert sleuths, and we have the credentials to back it up: six Grisham novels, dozens of episodes of CSI, hundreds of news stories on murders and rapes. But just like the professionals responding to a 911 call, we often come to conclusions about the victim’s identity and the nature of the crime based on the limited—and largely irrelevant—information directly in front of us.
Ask people to evaluate the academic aptitude of an elementary school student after playing them two video clips—one of her outside of school and the other of her taking an oral test—and the responses will shift based on the scenery in the first clip. When the student is shown in an urban, low-income setting, individuals view her inconsistent performance—getting some hard questions right and some easy questions wrong—and rate her ability as below grade level. When the exact same student is shown in a suburban, middle-class setting, they rate her ability as above grade level. Same girl, same performance, different conclusions. We hand out IQ points based on the size of her house and the number of trees in her neighborhood.
We can see the influence of the immediate situational context on how people assessed David. Finding him lying on the sidewalk in her upscale neighborhood, Claude Pritchett described him as “dressed nicely and not unkempt.” Yet, three hours later, the Emergency Department physician described David, now slumped in a hospital hallway, as “very disheveled, unkempt, his hygiene wasn’t the best. He looked dirty. He looked like our typical alcoholic.”
This also helps explain why the police officers didn’t give much thought to the possibility that the incoherent man lying on the sidewalk might have been the victim of a serious crime. The patrol service area that includes the 3800 block of Gramercy, with its generously spaced homes and landscaped yards, is one of the very safest in D.C. and had not recorded a single homicide the previous year. Although there were more than four thousand robberies in the forty-five patrol service areas in D.C. each month, David’s neighborhood averaged only two.
In the mad dash to understand the scene in front of us and decide how to react, a victim’s clothing, haircut, skin color, glasses, and perfume can all serve as signposts. In David’s case, one of the most significant cues was the vomit on his jacket. When interviewed after the fact, almost every person—from the Pritchetts, to the firefighters, cops, and EMTs, to the hospital staff—brought it up. And it seems to have had an immediate impact on people’s evaluations of him by triggering one of our most powerful emotions: disgust.
Disgust guides our lives to a surprising degree, altering our steps as we navigate the sidewalk (don’t step in that!) and steering us to certain seats on the subway. While different people experience disgust differently (interestingly, those with more conservative moral beliefs tend to be more sensitive), it’s a universal emotion. Disgust a Kazakh, Peruvian, Vietnamese, or your neighbor down the street, and chances are you’ll see the same telltale facial expressions: wrinkled nose, raised lips, open mouth. Disgust responses appear in kids at about the same age across cultures. In experiments, a two-year-old will generally eat what appears to be dog poop (actually a mixture of peanut butter and strong cheese), but a four-year-old will not.
If your stomach turned as you read about feasting on feces, you are not alone—the mere thought of something disgusting can produce the effect. And, in fact, disgust can be directed at a whole bunch of things beyond the physical world of maggot piles, pus-filled sores, and rancid hot dogs. We cringe at the thought of having sex with a pig, a child being beaten, or cannibalism at the Jamestown settlement some four hundred years ago.
Many scientists believe that disgust evolved to help our ancestors avoid parasites and microbes that were transferred through physical contact, primarily with food. But it also proved useful for navigating our social worlds, telling us which people and actions were appropriate and which to avoid. As a result, today we see evidence of both “core” disgust (triggered by rotting meat, rat droppings, and the like) and disgust aimed at social offenses (a wealthy man stealing from a church collection plate) in almost all cultures. Both help us stay “uncorrupted” or “pure.” But because the same areas of the brain may be recruited for both responses, sometimes things get mixed up: what starts as core disgust can result in feelings of moral disgust and vice versa. The implications for how we assess other people are jaw-dropping.
Imagine walking into a psychology laboratory to fill out a survey judging the appropriateness of various actions, like a friend lying on a job application, consensual sex between first cousins, or survivors of a plane crash killing and eating a mortally wounded fellow passenger. The desk you are asked to work at is sticky, and there is a plastic cup that appears to contain the remnants of a smoothie and a chewed pencil. Dirty tissues and greasy pizza boxes spill out of the overflowing trash can. If you are like most people, you would probably be a little annoyed and think that the university sponsoring the research should fire its cleaning crew. But surely the mess wouldn’t affect your answers on the survey—our sense of right and wrong, we assume, is fixed.
Yet when scientists conducted an experiment along these lines, they found that the filthiness of a room (or, in another version, the smell of fart spray) made people’s moral judgments significantly more severe. Disgust at the lab conditions generated disgust at the starving plane-crash victims.
Turning back to David’s case, we begin to see how this tendency might have come into play. The disgust that people felt upon smelling and seeing the vomit on his body may have caused them to keep their distance (remember the responding police officers who decided not to get involved, and the doctor who refused to work on David until he had been cleaned up). Assessing David’s injuries required close inspection, as did catching the clues that suggested a crime had been committed. No one who kept him at arm’s length was in a position to reach the conclusions that might have saved his life and quickly brought his attackers to justice.
Just as critically, the vomit may also have led the firefighters, EMTs, police officers, nurses, and doctors to engage in moral distancing. The physical disgust they felt may have generated an explanation for David’s condition that involved lack of discipline and poor character—drunkenness—rather than another potential cause: a stroke, seizure, diabetes, head injury, or drug interaction. And once the ETOH label was attached, David was in trouble.
From UNFAIR: THE NEW SCIENCE OF CRIMINAL INJUSTICE. Used with permission of Crown. Copyright © 2015 by Adam Benforado.
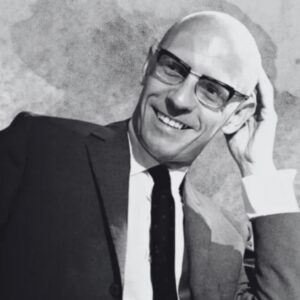
Adam Benforado
Adam Benforado is an associate professor of law at Drexel University. A graduate of Yale College and Harvard Law School, he served as a federal appellate law clerk and an attorney at Jenner & Block. In addition to Unfair, he has published numerous scholarly articles, and his op-eds and essays have appeared in a variety of publications including the Washington Post, the Philadelphia Inquirer, and Legal Times. He lives in Philadelphia with his wife and daughter.