On the Mysterious, Powerful Effects of Placebos
And What They Reveal About the Force of Hope
Mr. Wright
In 1957 psychologist Bruno Klopfer reported on the amazing case of a man he called Mr. Wright. Mr. Wright was suffering from advanced cancer of the lymph nodes. Tumors the size of oranges studded his skeleton and wound throughout his organs. He was so near death that he was more malignancy than man, his face pale on the pillow, an IV plunged into one of his stringy veins.
Some people, as they near the end of a long battle with cancer, their hair gone and their teeth loose in their sockets, are ready to exit, exhausted by the demanding treatments, by the burn of radiation and the poison of chemotherapy. But Mr. Wright, because he had a severe anemic condition, was not eligible for the treatments of the day, which were radiotherapy and nitrogen mustard. He had wasted away all on his own, without the help of cures that also kill. But his will to live, his desire to see the day, was strong, and the shadow of death that fell across his hospital bed, a dark hole into which he would soon dwindle and disappear, terrified him.
Then one day Mr. Wright—“febrile, gasping for air, completely bedridden,” according to his doctor—overheard people talking about a new cancer cure called Krebiozen, a horse serum, which was being tested at the very hospital he was in. Hope sprang up like a stalk inside him. He begged his doctor for a dose, and his doctor, although doubting the drug would help at this late stage, nevertheless loaded his syringe and took his patient’s wasted arm.
Three days passed as Mr. Wright lay quietly in his hospital bed. On the third morning after the shot of Krebiozen had been administered, his doctor returned to examine him, and an incredible thing had happened. Before the doctor arrived, Mr. Wright had swung his feet over his hospital bed and for the first time in months stood up straight on the floor, strong enough to support himself, to walk, even to stride, which he did, out of his room and down the ward to the station around which the nurses flurried. The doctor found this man who had been at death’s door now joking, flirting, cavorting. X-rays showed that the tumors had shrunk from the size of oranges to golf balls—having melted “like snowballs on a hot stove.”
No one could quite believe it, but no one could deny it either, because here was the man, once washed out but now ruddy with health and hope. Within ten days Mr. Wright was discharged from the hospital, cancer-free, and he went home to pick up where he had left off before cancer came to claim him, stepping back into his life as if slipping into a perfectly fitted suit. He was alive and loving it.
Days passed, weeks passed, and Mr. Wright remained free of malignancies. Within two months, however, reports came out in the news saying that the Krebiozen trial had concluded and the drug was worthless. Soon after that Mr. Wright’s tumors returned and he was back in the hospital, once more staring at the drain hole of death, at the shadow falling across his bed.
His doctor then did something that doctors today would never be permitted to do. He told Mr. Wright a story, a lie. The news reports, the doctor said, were wrong. Krebiozen was in fact a potent anticancer drug. Why, then, Mr. Wright wondered, had he relapsed, and so badly? Because, his doctor said, Mr. Wright had unfortunately been given an injection of the stuff from a weak batch, but the hospital was expecting a new shipment and it was guaranteed to be two times stronger than even the most potent Krebiozen to date. Mr. Wright’s doctor delayed administering anything to his patient so that his anticipation would build. After several days had passed, the doctor rolled up Mr. Wright’s sleeve; Mr. Wright offered his arm, and the doctor gave his patient a new injection—of pure water.
Again hope made an entrance. Mr. Wright let all his tumors go. Once again they shrank and disappeared until no trace of them could be found in his body, and once again he left the hospital. It’s not hard to picture him dancing his way through his days. A second remission! Mr. Wright lived for a further two months without symptoms and then, unfortunately for him, came another news report. The American Medical Association, after numerous tests on patients, issued its final verdict on Krebiozen, confidently declaring the drug to be useless. Mr. Wright’s tumors reappeared, and this time, within two days after his readmission to the hospital, he was dead.
The Pharmaceutical Factory in Our Heads
In the 1970s came the discovery of endorphins, which are opiate-like chemicals the body manufactures all on its own and which play a key role in the placebo effect, especially in cases of pain. The discovery led scientists to uncover a rich supply of nerves linking the brain to the immune system, which in turn resulted in the rise of a new branch of medicine called psychoneuroimmunology. Studies in this new medicine suggested that placebos may work to decrease pain—something they are especially good at doing—by increasing endorphins in the brain.
At the University of California, San Francisco, for example, in a 1978 double-blind experiment with young people who had recently had their wisdom teeth removed, most patients were given a placebo and reported significantly less pain. Then some of the subjects were given naloxone, a drug that is typically administered in emergency rooms in cases when a patient has overdosed on heroin or morphine. Naloxone works by blocking the opiate, thereby immediately reversing the effect of the deadly ingestion. In this study with the wisdom teeth patients, once they were given naloxone, the pain relief they had experienced as a result of the placebo suddenly vanished. Once again the young people were in pain. This outcome provided researchers with a strong suggestion as to how placebos might work. It must indeed be that they released the brain’s natural opiates—endorphins—and that as long as this release wasn’t blocked by naloxone, or by some other organic means, then these endorphins would allow us to find real relief.
Blue and Pink Pills
The form of the placebo has implications for its function. For instance, when it comes to pills, scientists have discovered that blue placebos tend to make people drowsy, whereas red or pink placebos induce alertness. In the 1970s several professors at the University of Cincinnati took 57 second-year medical students and divided them into four groups. Two groups received pink tablets and two groups blue tablets, and of the two groups receiving the same color, one group received one pill and the other group two pills. All of the tablets were inert. The students then listened to a one-hour lecture and after that went back to the lab to fill out forms rating their moods.
“The only thing we can say for sure is that 30 to 60 percent of the population can be fooled by a trick, by a sugar pill, by water, by an injection of saline or a bright pink sphere glittering in the palm.”
The results? The students who had received two tablets reported more intense responses than the students who had taken only one tablet. And of the students who had taken the blue tablets, 66 percent felt less alert after the lecture compared to only 26 percent of students who had taken the pink tablets. Medical anthropologist Daniel Moerman believes that the color of a capsule or a pill has a strong significance to the imbiber. Blues and greens are cool colors while reds and pinks are hot colors. A study in Texas showed that red and black capsules were ranked as strongest while white ones were weakest. “Colors are meaningful,” Moerman writes, “and these meanings can affect the outcome of medical treatment.” Blue pills make us drowsy while carmines perk us up. And large pills have more power over us than medium-sized ones, especially if they are multicolored.
The research on the size and color of pills makes one wonder if we might also be more strongly affected by pills embossed or engraved with a name: Tagamet, Venlafaxine, Zyprexa, Abilify, Concerta. Are drug companies not hoping that if they carefully and suggestively label their medicines, we will give their pills extra credence? Clearly the name matters. It is always multisyllabic and often suggests technological prowess. You cannot call a placebo Tim, for instance. The name should bring to mind test tubes and Bunsen burners with their petal-shaped flames. The name should also connote, somewhere in its utterance, the pure peace of good health, the abilities with which Abilify will endow you, the consonance of Concerta, when all the world makes solid sense.
Even more persuasive than pills, at least in the treatment of headaches, are placebo injections. A meta-analysis of a drug called Imitrex—which, when first introduced, was available only as an injection and then later as a capsule or a nasal spray—looked at 35 trials treating migraine sufferers with Imitrex versus placebo and found that, of those patients taking a placebo tablet, only 25.7 percent reported that their headache was mild or gone, compared to 32.4 percent of those treated with a placebo injection reporting relief. This may seem like a small difference, but it is statistically significant and could be expected to happen by chance only twice if the experiment were repeated a thousand times. Over and over, research has revealed that when patients are injected with an inert substance they report more pain relief than those who have simply swallowed a pill. Perhaps there is something about the needle, the press of the plunger as the supposed miracle liquid seeps below the skin and into the muscle, finding its way into the circulatory system, and at last to the wet red charm that sits within its curved cage. While a pill can be quiet, simple, its magic subtler and singular, there is drama in a shot.
Hope
Of course, none of this so far answers the question of exactly how endorphins get released in the first place. It seems to have something to do with belief, with hope, with faith. Even the smallest spark of it helps our heads to secrete chemicals so soothing that their analogues are illegal around the world. People who think they are drinking alcohol, but in fact are not, will nevertheless get tipsy. The opposite of hope is also very telling. Where it is absent, or unknown, medication sometimes fails to work. Valium, for instance, has been shown to affect a person only if he knows he is taking it.
But while there have been many studies done to predict the personality type of placebo responders, they have proven inconclusive. If only we knew! Then we would have a clear class of people to whom we could confidently feed inert substances and who could be assured of getting real relief. No such study, however, has been able to find a personality type, or rather, it would be more accurate to say that all of the studies conflict with one another. Some claim that people who respond to placebos have neurotic personality types; others claim that introverts are more likely to be fooled by placebos; while research from Britain has found that extroverts are the group most susceptible to placebos. Scientists have claimed at different times that placebo responders are both quiet and ebullient; that they have poor ego formation and superegos the size of a city; that they are judgmental as well as easily swayed; that they are trusting and skeptical. The net sum suggests that there is no definitive profile of a person likely to respond to a placebo. Everyone is a responder—maybe not all of the time but some of the time, in some situations, in great pain or fear, perhaps, or with wants so large that they outstrip the self who holds them. We do not know. The only thing we can say for sure is that 30 to 60 percent of the population can be fooled by a trick, by a sugar pill, by water, by an injection of saline or a bright pink sphere glittering in the palm.
*
Almost four centuries ago, René Descartes hypothesized that the soul was located in the brain’s pineal gland, a tiny structure in the shape of a pine cone lodged deep in crenelated paste. By separating the soul into its own space, Descartes gave birth to the mind-body problem. But no one really thinks anymore that there are two separate entities known as mind and body. We know—do we not?—that we are all body and that being all body is an astounding, miraculous, never-ending curiosity and weight. We know that all our tangles of emotions, whether arising from seeing a sunset or contemplating suicide, are neurochemical phenomena. It’s all about synapses and liquids coursing through our heads. And yet these very real, very visceral human hurts can be healed by a gentle hand on top of our own, by a math professor who likes to listen. Something about the telling of stories can make our miseries bearable, and is this not in essence what a placebo response is? “Placebo” comes from the Latin for “I will please” and when our math professor puts down his chalk and sits in his rumpled suit and listens with his head cocked slightly to one side, the person on the other side is pleased. He is placeboed. And he is helped.
A placebo is not just a sugar pill. A placebo can be an event as well as a thing. Anytime a person endows something with meaning, whether it’s a relationship or an occurrence, he is held in a warm embrace; he is helped by something that does not exist except as dream or hope or expectation. Much of the power of the placebo comes from the one who is hurting, which means we can start to see the sheer energy in states of sickness—what we are capable of doing when down and supposedly out, how strong we really are, even in our weakest moments, with our brain always ready to find us some faith.
__________________________________
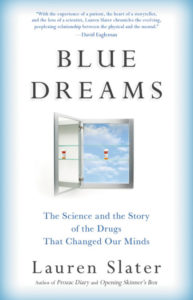
From Blue Dreams. Used with permission of Little, Brown and Company. Copyright © 2018 by Lauren Slater.