Why Are We Compulsively Drawn to Watching Our Newborns Sleep?
Michael J. Stephen Considers the Physiology and Philosophy of Breathing
Sometime after midnight, one deep January night, I remember walking into my bedroom and staring down at my first child in her crib, born on New Year’s Eve and now barely two weeks old. The silver moonlight poured in through the window, illuminating her outline. Her eyes were closed tight, her arms thrown over her head as if in an eternal stretch, her head tilted slightly to the right. Her intoxicating newborn smell brought rapture and calm.
Like millions of parents before, I considered the serenity of a newborn’s sleep, its restorative depth, but I also instinctively checked on function, to make sure life still blazed within despite the outward calm. This meant checking her belly, to make sure she was breathing. Of course she was: her chest and abdomen moved up and down under her blanket in the rhythmic flow we all recognize as life.
When we observe our loved ones sleeping, old or young, human or pet, we are instinctively drawn to their breath. There is something essential in it we are all attuned to, something we both automatically and unconsciously equate with life. Each time we check on each other, we are validating the words of the Roman philosopher Cicero, dum spiro, spero, “As I breathe, I hope.”
Physiologically, what we are observing is the miracle of gas exchange, taking from the atmosphere an invisible element and bringing it into our body to be consumed. The process begins with a signal from the brainstem, the primitive part of the brain at the base of the skull, which travels through nerves down to the muscles of inspiration, instructing them to contract. The biggest and most important of these muscles is the diaphragm, a thin, dome-shaped sheet of skeletal muscle that separates the thorax (chest cavity) from the abdomen.
With each signal, the diaphragm contracts downward, pulling the thoracic cavity and the lungs with it. This creates negative pressure in the trachea and lung tissue, and with this negative pressure air rushes in, just as water flows down a river. Entering through the mouth or nose, the air travels down the back of our throat, past the vocal cords, and into the trachea. About halfway down the sternum, the trachea divides into the left and right bronchi, which divide again and again into lesser bronchi, termed bronchioles. The air moves through the bronchioles, which extend deep into the lungs, like tendrils from a star erupting in space, until finally it penetrates into cave-like recesses, deep in the lungs. Known as alveoli, and resembling cells of a honeycomb, these grapelike clusters at the end of the increasingly narrow breathing tubes are where gas exchange occurs.
Like millions of parents before, I considered the serenity of a newborn’s sleep, its restorative depth, but I also instinctively checked on function, to make sure life still blazed within despite the outward calm.
Continuing its natural flow from an area of high concentration to one of low concentration, oxygen moves effortlessly through the thin surface of alveoli, just a single cell thick, to the adjoining capillaries. Here, thousands of hungry red blood cells grab oxygen, and together they are pumped by the heart to the arteries and then to the tissues of the organs, which are infiltrated with a vast network of capillaries. At the tissue level, oxygen hops off the red blood cell and diffuses through the capillaries into the cells of whatever organ or muscle is nearby.
Within each cell are mitochondria, the specialized organelles in which cellular respiration takes place: oxygen joins with glucose to produce carbon dioxide, water, and adenosine triphosphate (ATP). ATP is our primary source of energy, the molecule that drives many of our bodily reactions, including muscle contraction, enzyme production, and the movement of molecules within our cells. ATP causes these reactions by breaking off one of its phosphate groups, whose electrons are in a high-intensity state, and transferring this energy to drive the necessary processes of the cell. Now adenosine diphosphate, it gets recycled back to the mitochondria to become high-energy triphosphate again through the ongoing process of cellular respiration.
A byproduct of oxygen use and cellular respiration is carbon dioxide (CO2), which diffuses out of the cell, into the blood, and back into the capillaries, which now flow to veins. Not used by our body, CO2 is shunted back to the lungs by our venous system, where it diffuses into the alveoli. From there, the air, with its new mixture of gasses, is pushed out through the network of bronchioles and bronchi as the diaphragm relaxes with exhalation, and ultimately expelled out of the mouth or nose and back into the atmosphere. The CO2 disperses easily into the air, where its levels are very low at 0.04 percent of atmospheric gas. Levels of oxygen in the atmosphere stand at a comparatively robust 21 percent, so on our next breath we are able to fill up again with this molecule of life. (The rest of the atmosphere is almost all nitrogen, harmless to us but also useless.)
We are attuned so closely to this process of inhalation and exhalation in our slumbering loved ones because we have an instinctive understanding of its urgency: while we can skip meals, breathing must be continuous. The system must be finely coordinated as gas levels need to be kept within a very narrow range in our blood. Receptors in our aorta and carotid artery continuously monitor levels of oxygen and carbon dioxide and send feedback to the respiratory center in our brainstem. Even the slightest change in the levels of gas will trigger more signals or fewer to go out to our muscles of inspiration. The activity in the respiratory center of our brainstem also feeds back to our cerebral cortex, or higher brain, making us aware of any impending danger. This creates the alarming sensation we are all familiar with if our brain senses something wrong with our oxygen or carbon dioxide levels, as when we hold our breath.
Carbon dioxide is what causes most of the initial problems when we hold our breath, because as it builds up in our blood during a breath hold, it begins to break down into acid. This acid is toxic to our cells, especially as it begins binding with proteins and other molecules it shouldn’t, impeding the normal function of cells. As the breath hold continues, lack of oxygen also becomes a problem, and as cellular respiration in our mitochondria ceases with the dearth of oxygen, cellular death ensues. The cells of the heart muscles are especially sensitive to this, and cardiac arrhythmias can ensue in extreme cases of too much carbon dioxide or too little oxygen. Breathing is the most important thing we are aware of doing, and the body regulates it tightly.
We are attuned so closely to this process of inhalation and exhalation in our slumbering loved ones because we have an instinctive understanding of its urgency: while we can skip meals, breathing must be continuous.
The foundation of our understanding of these pulmonary processes, and indeed of all Western medicine, was laid in ancient Greece. After the mythical Apollo and his mystical son Asclepius, whose rod is the symbol of medicine today, the first legendary but real figure in the history of medicine was Hippocrates, born in 460 BCE on the Greek island of Kos. He is forever known for creating the oath that all physicians still recite when they receive their diploma, and is deservedly known as the Father of Medicine for his insight that disease was the consequence of natural processes and not the work of magic or the gods.
In addition to contemplating many other anatomical systems, Hippocrates studied breathing. He recognized that the inhalation of air was fundamental to life. For this reason, Hippocrates and the Greeks viewed air as something vital and transcendent. They called it pneuma, which literally means air or breath but for the ancient Greeks also meant life force. This pneuma was inhaled and then passed through the lungs, into the blood, and on to the heart, where it became the pneuma zoticon, or vital spirit. This vital spirit was then carried to the organs, including the liver and brain, where it was transformed into pneuma psychicon, or animal spirit, which was considered the driving force, created by the body from air. From spirit (air or pneuma) to vital spirit to animal spirit, the Greeks and Hippocrates insightfully saw the essence of our existence as a continuum from the atmosphere.
Some five hundred years after Hippocrates, Claudius Galenus was the next great figure to change how we think about breathing and circulation. Better known simply as Galen, he was born in September 129 CE, in the Aegean Sea town of Pergamon, part of modern-day Turkey. His father, a wealthy patrician, originally had plans for his son to become a philosopher and statesman. These plans changed when the father dreamed that the mythical physician Asclepius visited him with a decree that his son study medicine. Galen’s father spared no expense, and Galen was educated at the best institutions throughout the Roman Empire.
Some five hundred years after Hippocrates, Claudius Galenus was the next great figure to change how we think about breathing and circulation.
When he finished his studies, Galen settled into practice in Pergamon. He became the personal physician to the gladiators of the high priest of Asia by performing an act of daring. According to his own report, he eviscerated a monkey and then challenged the other physicians to repair the damage. When none stepped forward, he did the surgery himself, successfully restoring the monkey and winning over the high priest. He later moved to Rome and became the personal physician to several emperors, most notably Commodus, who reigned from 161 to 192 CE.
Galen contributed to many areas of medicine, and added to our understanding of the lungs and circulatory system. He noted that “blood passing through the lungs absorbed from the inhaled air the quality of heat, which it then carried into the left heart.” Human dissection was prohibited by Roman law, but Galen dissected both primates and pigs. He was the first to describe the two separate systems of circulation, the arteries and the veins. He believed that the liver, with its dark purplish interior, was where blood originated. From the liver, he postulated, half of the blood went out to the veins and was delivered to the tissues and consumed. The other half went to the lungs via a vein, where it picked up pneuma, then on to the heart, the arteries, and then the tissues.
Although Galen’s theories on blood flow would be proven to be partially wrong, he was important, like Hippocrates, because of his methodology. Galen cemented the notion that medicine and disease were not the products of divine intervention from the gods but could be discerned from empirical evidence and deduction based on observation and cause and effect. Nonetheless, more than a thousand years passed before his ideas on the movement of oxygen within the blood’s circulation were corrected.
__________________________________
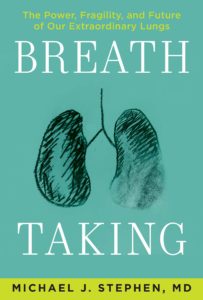
Excerpted from Breath Taking © 2021 Michael J. Stephen. Reprinted with the permission of the publisher, Atlantic Monthly Press, an imprint of Grove Atlantic, Inc. All rights reserved.
Michael J. Stephen
Michael J. Stephen, MD, is the author of Breath Taking: The Power, Fragility, and Future of Our Extraordinary Lungs. Dr. Stephen is an associate professor at Thomas Jefferson University in Philadelphia, and director of the Adult Cystic Fibrosis Center. He is a leader of numerous clinical trials and has been on the front line caring for COVID-19 patients—and also recovered from the virus himself. Over the past two decades he has studied advanced end-stage lung diseases and worked with patients at diverse locales, including a Massachusetts prison hospital and a pediatric HIV clinic in Cape Town, South Africa. A graduate of Brown University and Boston University Medical School, he lives in New Jersey.