Panacea or Problematic Hype?: The Uncertain Promises of Ketamine Therapy
Andy Mitchell on Psychedelics and the FDA's Controversial Shift in Defining Clinical Depression
For my first trip I would receive a “super-dose” of ketamine intravenously while having my brain scanned in a 3-Tesla fMRI machine. Unless I was lucky, in which case it would be a high dose of dimethyltryptamine (DMT), lying between the large rings of a PET (positron emission tomography) scanner. This was the psychonautical equivalent of a three-star Anthology meal at the Fat Duck, or a performance of Beethoven’s Seventh by the Berliner Philarmoniker, if the meal were eaten standing up in an airplane toilet, the concert heard over the mêlée of Black Friday on Oxford Street.
Ketamine: special K.
“It’s a mong for end-stage burners,” said Palmer, techno DJ and medicinal gourmand. “I could play Abba and no one would clock it.”
“It’s a horse tranquilizer,” said my drug-naïve mum. “Those Thai soccer boys took too much and got stuck in a cave for days.” (She’d only heard about the Netflix documentary.)
“I think the rescue team gave them it to stop them panicking, Mum.”
“It’s a Swiss Army knife,” said an anesthetist colleague, “used off- label as an anti-inflammatory, for pain relief, for neuroprotection, as well as an anesthetic in surgery and critical care.”
I’d also read about anti-aging hacks in California “playing” with mega-doses that led to a complete collapse in space–time coherence, a few minutes stretching out to a “felt” century. I would be catheterized for the best part of an hour. It might be that the first human to live 5,000 years (me) had recently turned fifty and already had flattening arches and an arthritic hip.
I’d also read about anti-aging hacks in California “playing” with mega-doses that led to a complete collapse in space–time coherence, a few minutes stretching out to a “felt” century.
These perspectives layered my ketamine “set”—my “priors,” to use the jargon of the neuroscientist, meaning the beliefs one holds before any experience has taken place, and the tendency for those beliefs to shape the experience itself.
The study was being conducted by Imperial College’s Centre for Psychedelic Research, an international leader, and one of the first groups to be established with seed money from the philanthropist/ investor/podcaster/author Tim Ferriss, of The Four-Hour Work Week, The Four-Hour Body and The Four-Hour Chef, fantasies of compression enabled, I imagined, by the 4,000 years he’d spent exploring these things in psychedelic space-time. I had just received the patient information sheet (PIS), following a two-hour interview with one of the research assistants that had covered my psychological history, my educational history, my relationship history, my drug and alcohol history. And this was just the pre-screen.
In the days to come I would have a formal clinical interview lasting several hours with a consultant psychiatrist. It made sense to be careful about who one loaded in the barrel of an MRI scanner and shot into unimagined realms. In most psychedelic trials there were general criteria for “healthy”: no history of suicidality, psychoses, bipolar, personality disorders or long-term drug addiction. And for this particular trial there were extra criteria: that I was both ketamine-naïve and hadn’t been near psychedelics in three months, the latter being why I had elected to make ketamine the first of my ten trips.
The PIS was long, detailing every stage of the investigation in language that was supposed to be accessible to the layman to ensure the study’s safe passage through the ethics committee. It didn’t begin promisingly: “Detecting synaptogenesis induced by Ketamine/ Dimethyltryptamine and motor learning using the tracer [11C] UCB-J in an integrated PET-fMRI paradigm.”
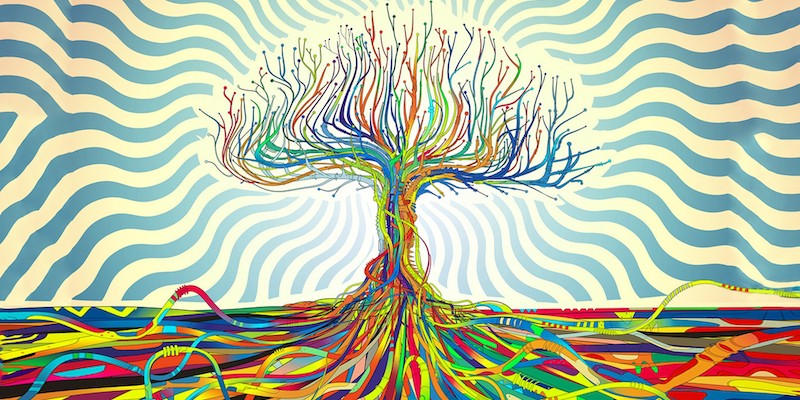
“The brain’s ability to reshape and make new connections during adulthood,” it continued, “is essential to our ability to learn new skills and form and access memories. This process, broadly described as neuroplasticity, can be disrupted by many different factors and is increasingly believed to be centrally involved in a number of mental health disorders and cognitive impairments.”
This related to the “synaptogenesis” part of the title. New experiences may be registered in the brain by the generation of dendritic spines which sprout, tree-like, on one end—the dendron—of the neuron. The language of neuroplasticity is infused with the metaphor of the tree: the sprouting is called “arborization” after the Latin; under high magnification the dendrites look like foliage.
New Age psychedelic therapists like the recently disgraced Françoise Bourzat take the metaphor a stage further, seeing in the images of tripping brains anatomical symbols of the plants or mycelial (fungal) networks that inspire them. To the more circumspect this might be no different from getting high and seeing the profile of Donald Trump’s quiff in wispy clouds.
Most neuroscientists would think of both as examples of pareidolia, the tendency to perceive a specific, often meaningful image in a random or ambiguous sensory pattern. Bourzat’s gloss on ancient human-plant synergy works less well for ketamine, which has no botanical basis but was developed in 1962 in a Detroit lab owned by a subsidiary of the pharmaceutical giant Pfizer: a little more difficult to romanticize than Mazatec mushrooms and Amazonian vines.
Neuroplasticity has for decades been one of the most popularized areas in neuroscience, long predating the current interest in psychedelics. “Rewiring” has become part of the vernacular of life coaches, football managers, schoolteachers and mobile apps. (One might describe its recent ubiquity as the “Joe Dispenza Effect,” after the chiropractor-turned-neuroplastic guru.)
Plasticity is seen as a “hack” allowing us to acquire new skills and knowledge, change old patterns or “priors,” re-think ourselves. (Today Joe’s tweet reads: “To create a new personal reality—a new life—we must create a new personality. We must become someone else.”) This mode of understanding makes it inevitable that plasticity and psychedelics are saddled together: two “new” instruments of improvement, passwords for the near-limitless possibilities of self-transformation, couched in the sexy-sounding language of neuroscience.
Keen to learn something of what might be about to happen to my brain, I run a Google search for “evidence of imaging of synaptogenesis.” It yields little. A few lead-in adverts (dictated by the engine’s plastic algorithm) for how to train your brain to give up sugar or “speak proper grammar,” then a low-res black and white clip lasting a few seconds that resembles the beginnings of cinema: dendrites like tiny forks of lightning across a night sky, appearing, then disappearing, then appearing again, until they stabilize. This was arborisation alright, but in larval jellyfish.
In clinical neurology, the field I work in, there’s a different emphasis on neuroplasticity. It’s understood not as “growth” or “transformation,” but as the mechanism of repair or compensation after devastating injury. The tone is different too, of course: more circumspect, less certain, at least as far as hard evidence goes. The effects of plasticity are seen clearly on brain scans taken at different intervals after a traumatic injury, for example, but its mechanisms, and the extent of its capacity to restore the injured brain, remain vague. At present there are no commonly used drug interventions with the power to significantly promote it.
But it remains a term in daily use. Every trauma patient will, after they are sufficiently reoriented in space and time, be given a basic lesson in the brain’s ability to heal itself: that the restoration of lost speech, a paralyzed leg, amnesia, an altered personality, depend on old pathways being restored, or compensatory pathways being forged. Some patients make complete recoveries, many don’t. Most clinicians cite two years as the length of the window in which such changes might be seen in the adult brain. A few make it longer, three to five years; a few are more conservative, confining the window to eighteen months.
It’s also a way of distracting everyone (including the clinicians) from the terrible reality of how little can be done medically for the patients, how a significant percentage of their recovery remains in the lap of the gods.
In the absence of detailed evidence, this becomes a matter of convention rather than science. It’s also clinically strategic, something to give the patient and her family hope, the motivation to rehab, to keep emotional devastation at bay for as long as they remain “in” the window. In this context plasticity is often more a matter of faith than science. It’s also a way of distracting everyone (including the clinicians) from the terrible reality of how little can be done medically for the patients, how a significant percentage of their recovery remains in the lap of the gods. Then the window closes.
The PIS continued, “In depression, connections between regions involved in cognitive, emotional and memory processing appear to be weaker, and the brain’s ability to form new connections in these regions also seems to be reduced.”
Imperial is now widely known for psychedelic imaging in the field of mental health. Since the first wave of research there in the Fifties and Sixties, advanced neuroimaging technologies have been developed which can map the effects of psychedelics on specific areas of the brain.
One of them is the default mode network, a collection of structures in the mid-brain associated with mind-wandering, remembering the past and planning for the future—all those self-referring thoughts that demand their thinking. Another is the salience network: interconnected regions of the brain that select which stimuli are deserving of our attention. Some kind of dysregulation in these networks is thought to be associated with the experiences of “meaninglessness,” the negative appraisals of self and mental rigidity that are symptomatic of clinical depression.
To date, much of the neuroimaging research has depended on observing general changes in levels of activation across these networks following psychedelic treatment. Plasticity, which happens at the level of individual neurons, has been inferred rather than observed directly. The Imperial study I was being screened for aimed to take this a stage further. Combining fMRI imaging, which offers the precise location of activated areas, with PET scans, which allow any changes to be tracked across time, the intention was to observe synaptogenesis as it was happening. As per the PIS, “there is a growing amount of evidence suggesting that ketamine’s antidepressant action may stem from temporary enhancement of neuroplasticity in important areas.”
A quick search of the literature suggested that most of the “growing” evidence was indeed inferred rather than directly observed, based on changes to larger patterns of brain activation or to neurochemistry. The only other evidence comes from animals: a couple of studies reported growth of dendritic spines in rats. But there are limits to translating rodent psychiatry: however grim it might be to spend your entire, brief life confined to an environmentally impoverished cage, the rat cannot be meaningfully diagnosed with depression or other human mental health conditions.
The lack of direct evidence reflected something of how provisional and callow much of the neuropsychiatric research on psychedelic therapy was. Even so, the current study was groundbreaking, using state-of-the-art technology in a clinically relevant area of investigation, and at the “hard science” end, compared to the vast majority of therapeutic research. It would also be eye-wateringly expensive: running scanners over multiple sessions with all the adjacent tests and staffing requirements meant the cost, even with a cohort of fewer than ten volunteers, would run into the high six figures.
The finance and science of psychedelic medicine are complexly entwined. In 2013 the US Food and Drug Administration (FDA) designated a variant of ketamine a “breakthrough therapy” on account of its apparent ability to reverse the acute symptoms of “treatment-resistant” depression. This led to a pharmaceutical arms race, the details of which were explained to me by Josh Hardman, founder of Psychedelic Alpha, one of the most reliable sources of financial information and commentary on the nascent psychedelic “sector.”
“Ketamine has been used ‘off-label’ for a number of years in the treatment of depression,” he told me, “but according to the calculus and playbook of pharma there’s little ‘defensibility’ in these cases: it’s not patented in any meaningful way for these uses, so there was no prospect of digging a meaningful IP moat around it.”
This changed in 2013 when the pharmaceutical company Janssen decided to use what Hardman called a “textbook procedure from the pharma playbook” to bring a variant of ketamine to market with patent protection. It chose one variant, s-ketamine (or “esketamine”), and partnered it with a specific drug-delivery mechanism, in this case a nasal spray. They then sought and achieved patent protection from the relevant government body on the intranasal administration of esketamine in treatment-resistant depression, under the trade name Spravato.
In other words, certain design choices that had little to do with empirical evidence allowed them regulatory exclusivity on their variant and permitted them to market it as a “new chemical entity.” This type of “innovation,” commonplace in the broader pharmaceutical industry, is, Hardman suggests, now entering the psychedelic sector.
In other words, certain design choices that had little to do with empirical evidence allowed them regulatory exclusivity on their variant and permitted them to market it as a “new chemical entity.”
But Janssen ran into significant problems with the health economics of its “invention,” as the price was forced up to $6,785 for a month of treatments twice a week. “Remember,” explained Hardman, “ketamine, unlike other psychedelic interventions, is associated with ‘temporary’ changes in neuroplasticity; meaning that its prescription has a different economic model than ‘one-off’ treatments.” Then, he went on, there was the fact that there was little long-term evidence for its efficacy. “Some experts, like former FDA reviewer Erick Turner, were flagging that even the more short-term data showed only modest efficacy and raised some concerns over patient safety.”
These factors have meant that even if Janssen is able to convince healthcare systems that it has a product with a novel mechanism of action, the cost and lack of evidence make it very difficult to produce a convincing economic case for a health authority, especially in the U.K., where NICE (the National Institute for Health and Care Excellence) has a cost-effectiveness requirement for recommending treatments for the NHS. Meanwhile, Hardman told me, Canada had flat-out refused to grant Spravato data protection, the Canadian court finding that it did not warrant the designation of “novel compound.”
Such limitations do not obtain in the U.S. The FDA’s initial approval of esketamine involved loosening its definition of “treatment-resistant depression.” Previously this diagnosis had been restricted to those who had tried two classes of antidepressant medication (there are several, including SSRIs, SNRIs, tricyclics). It changed this to mean any two different pills: i.e., it could be the same class of antidepressant, as long as over the course of their depression history the patient had taken two different brands. Given the whims of prescribers and patients, this sets a very low diagnostic threshold.
Despite this, the initial FDA approval remains, and much of the subsequent clinical research has adopted the same criteria for treatment-resistant depression. Even with such low-hanging fruit, Hardman told me, Spravato has not quite been the blockbuster Janssen had hoped for, though it remains lucrative by most standards, just not by pharma standards: by 2029, Global Data predicts, it will generate world sales of approximately $383 million.
______________________________

Excerpted from Ten Trips: The New Reality of Psychedelics by Andy Mitchell. Used with permission of the publisher, Harper Wave. Copyright 2023 by Andy Mitchell.
Andy Mitchell
Andy Mitchell is a neuropsychologist, therapist, and the author of Ten Trips: The New Reality of Psychedelics. He has specialized in treating patients with rare brain conditions, head injuries and epilepsy, and in the application of mindfulness for neurological patients. As a therapist he has worked with people with a range of mental health disorders. Before entering medicine, his first degree was in English Literature at Oxford University. He is originally from Leeds.