Kidneys, Twins, and Pathological Optimism: The Story of the First Successful Organ Transplant
Brandy Schillace on Dr. Joseph E. Murray's Groundbreaking Surgery
“We didn’t think we made history. We didn’t even think of history. We thought we were going to save a patient.”
–Dr. Joseph E. Murray, transplant surgeon
*
December 20, 1954, dawned to thick falling snow. By midafternoon, Dr. Joseph E. Murray, a surgeon at Harvard’s Peter Bent Brigham Hospital in Boston, stood in his kitchen with an ingredient list for eggnog. A balding, pleasant-faced man, Murray and his wife, Bobbie, were preparing for their annual Christmas party, 75 guests strong—but the phone rang in the hall before he could crack the first egg. “It’s the pathology people,” Bobbie told him. They both knew what that meant. Murray dropped his whisk and threw on his coat. He cranked the engine of his car, swerved out of the drive and onto icy roads. The Brigham Pathology Department had a cadaver for him.
It’s not often that a surgeon springs into action for the sake of a patient already expired. But Murray wasn’t thinking of the corpse. He thought instead of a young Coast Guard member named Richard Herrick, who that December lay in fits of toxicity-induced psychosis in the final stages of renal failure. Murray did not want the cadaver for its organs, a natural assumption in an age when Western medicine has proven its ability to extend life through spare parts. But in 1954, there were no spare parts; no organ transplant had ever been performed successfully. At least, not yet.
If a kidney could be moved, alive, from one body to the next, why not a heart? Why not a lung?
As the Christmas party went on merrily without him, Murray would spend the evening taking apart a fresh cadaver, painstakingly isolating and then removing a kidney—then repeating the process in reverse and putting the organ back in. It made no difference to the departed patient, but in three days’ time, these hours spent in surgery might mean life or death; this was practice. On December 23, Murray and a team of fellow medical mavericks would subject Richard Herrick’s brother Ronald, a Korean War veteran, to a dangerous surgery: they planned to remove one of Ronald’s healthy kidneys and give it to Richard. It was to be the first transplant surgery of its kind and would inspire a race to other firsts. If a kidney could be moved, alive, from one body to the next, why not a heart? Why not a lung? For Robert White, a young medical student in the shadow of Murray’s operating theater, the surgery would spark a singular and ambitious idea about bodies and their brains.
*
The human body is a messy, shifting organization of constantly dying and regenerating cells. The parts are the whole, and the slightest disruption can introduce a cascade of cell death. Consider your lungs: they must provide your brain with oxygen, or the brain will die. Yet your brain is necessary for engaging respiration. No brain, no breathing; no breathing, no brain. This same interdependence is true right down to the cellular level. When we die, we die all over, and for most of human history, the failure of even a single organ was effectively a death sentence. It’s not that medicine hadn’t tried to save organs and extend life; it’s that it had tried and failed.
By the late 19th century, the introduction of antiseptic to combat germs, cleaner means of treating wounds, and neater ways of sewing sutures meant that surgery could be practiced with reasonable safety. With dependable anesthetic and much lower chances of infection, the surgeon could cut more deeply into the body cavity than he would ever have dared before. He could, in other words, do more than merely cut visible tissue, remove obstructing tumors, or carve off a limb; a skilled surgeon could correct the body, set compound fractures, and, in severe cases, operate on the organs themselves, to extract a burst appendix or perform a mastectomy, for example. But despite these (albeit grim) successes, removing any organ damaged it beyond repair. You could take out one that ailed a patient, but you couldn’t pluck out a healthy one to give to someone else. Organs are fed by expansive networks of delicate blood vessels, and what you cannot “revascularize”—suturing torn vessels together without leakage—you cannot preserve. Transplant science could never progress unless this hurdle could be overcome. And as with most early attempts, the first experiments in doing so were messy, macabre, and almost universally subject to failure.
When we die, we die all over, and for most of human history, the failure of even a single organ was effectively a death sentence. It’s not that medicine hadn’t tried to save organs and extend life; it’s that it had tried and failed.
Alexis Carrel, a French surgeon and Nobel laureate, performed most of his surgeries on animals, particularly dogs. Revascularization only became possible in 1894 thanks to Carrel’s experiments with silk ligatures; the fibers were fine enough that, aided by sewing lessons from an embroiderer, Carrel could patch up blood vessels with stitches so small they could scarcely be seen with the naked eye. To avoid puncturing the vessel, he folded its tiny ends like a shirt cuff, stitching end to end so the blood would only come in contact with the vessel walls. Once he perfected the technique, he set his sights on transplanting a dog’s kidney. He had long been interested in treating kidney disease; patients regularly died of renal failure, and to stall that end, Carrel proposed experimental surgery. After all, you could remove one kidney without damaging the other, and—since the bean-shaped organs produce urine as a by-product of filtering toxins from the body—you could easily tell if your transplant succeeded by measuring urine output. The cutting out worked pretty well. The putting back in was a more complicated matter.
Through his work with the vascular system, Carrel understood that the secret to keeping a kidney alive had everything to do with blood supply. One of his first trials involved the removal of a dog’s kidney, which he kept isolated and artificially infused with blood in his lab before putting it back into the dog. When he put the kidney back into the same dog, it usually began working again, and the dog and kidney lived on just fine. But when he tried putting the kidney into a different dog, death usually followed. Not only did the transplant fail, its failure killed the host as well, as infection from the dying organ spread. Curious about the processes involved in this decay, Carrel performed the first of a strange and macabre series of experiments, swapping the limbs of dogs. Now living and working in New York, he opened the thighs of two dogs, one white and the other black. Soon, they wore each other’s limbs.
Carrel told a colleague that such work was far simpler than organ transplants, though to unite the femurs to the socket he had been forced to ram a nail through the marrow cavity. The surgery caught the public’s imagination, and fanciful sketches appeared in the Washington Post, giving the impression that the dogs had run about sporting their new limbs. In fact, they were never even able to move the new limbs—their nerve tissue grew back much too slowly, and after ten days, the dogs’ legs grew fetid and rotten. Both animals ultimately died of infection. More trials followed, and more failures, too, the reason for which would not be discovered until 1924. This time, the breakthrough belonged to one Emile Holman, a surgeon who worked for Brigham some 25 years before Joseph Murray.
The cutting out worked pretty well. The putting back in was a more complicated matter.
Holman’s interest was in skin transplants, which had already been used to some effect for 50 years. As industrialization increased faster than workers’ rights, accidents were common and often severe. In 1878, a laborer named Samuel Root suffered vicious burns in an iron molding factory when a stream of liquid metal ran across his foot; other unlucky workers became caught in machines and had clothes and skin ripped away. With enough of the body’s protecting layers of skin burned or missing, a patient would die—and many did. However, a few surgeons risked trying to cover wounds with additional skin in hopes that they would heal over. Historian Susan E. Lederer even recounts tales of superannuated 19th-century surgeries where skin from two hundred different people combined to rebuild a single woman’s scalp, a quilt of humans with the stitches still showing. But as with all other transplants of the time, skin grafts never took for long. They puckered, pulled away, and died. Sometimes they held on long enough for the patient to recover their own skin; usually, they did not, and pain and infection ensued.
Blood typing had gained credence throughout the 1920s and 1930s, and by the 1950s had been almost universally accepted. This still-developing science gave Holman an idea. The allograft, or transplant of healthy skin from one person to another, had never been successful—not for long, anyway. But in Holman’s day, children, with their grasping fingers above hot stoves and stumbling toes near open fires, were frequent burn victims. Perhaps a parental match would be almost as good as using the child’s own skin, he thought, and so harvested grafts from a burn patient’s mother. The thinking might have been sound, but those grafts failed, too. Worse still, each time he replaced the child’s allograft, it failed faster than before. The “destroying agency,” Holman realized, came from the body itself.
Soon after, James Barrett Brown, a St. Louis plastic surgeon, confirmed Holman’s fears: the “agent” was, in fact, an immune response. Somehow, the host body recognized foreign tissue, perceived it as an invading threat, attacked, and rejected it. The body seemed to know where it began and where it ended, and would accept no alien flesh. This meant sure failure for anyone hoping to transplant skin (or anything else) from another’s body, a notion that, by 1940, had come to be accepted as fact.
By 1950, Leo Loeb, a high-profile and prolific New York biologist, declared transplant prospects “hopeless” and a complete “waste of time.” His pronouncement seemed to be the death knell of transplant science for those practicing in the United States. And yet, at Peter Bent Brigham Hospital, the study of transplant continued. The hospital’s surgeon in chief, Francis Moore, still believed there must be a way forward—and he brought Joseph Murray on board as an enthusiastic kindred spirit. Harvard’s leading medical men looked on in pity and derision at what they considered the misguided captains of the university’s very own ship of fools.
Then 32 years old and fresh from his training in plastic surgery, the young Dr. Murray remained unflappable about the possibilities. “I have been accused of being a pathological optimist,” he would write in his memoirs years later. He called his work in transplant “surgery of the soul”—it gave his life a sense of purpose, and no fear of skeptical colleagues would do much to shake his confidence. He repeated Carrel’s dog experiments—all except for the leg swap-and even transplanted cadaver kidneys into sick patients by inserting them into the thigh, where the bulge would be less noticeable and closer to the vents for urine. The point of such an operation wasn’t true transplantation; a thigh kidney could filter toxins, but Murray knew the organ would eventually fail. The hope was simply that an extra kidney might take the strain off the beleaguered pair belonging to the patient, even for a short while. In most cases, however, it bought the patient only weeks, or days. Murray believed there must be a way to make the transplants work longer, but with 100 percent rejection rates, no one dared a full human trial. At least, not until Richard Herrick turned up at Brigham’s emergency ward.
Richard had been an active and healthy 22-year-old serving a tour aboard a Coast Guard vessel traversing the Great Lakes. In the fall of 1953, however, he fell suddenly ill, suffering weakness and dizzy spells. The crew sent him ashore, but his condition held on like a bad flu. Then, in January 1954, he woke to swollen legs and ankles. At first the problem was intermittent, and would gradually diminish throughout the day. But as the months wore on, the swelling continued through into the evening, the hot, tight skin making it difficult for Richard to walk. The pain sent him to see doctors, who diagnosed an excess of protein in his urine. It was a worrying sign: his kidneys were struggling to properly filter waste. Soon Richard’s energy began to drain away; his mouth tasted strange and metallic, and he suffered from constant nausea and vomiting. Then, his urine ceased to flow. Richard was in renal (kidney) failure.
Our kidneys filter 200 quarts of blood in a single day, separating out toxins like urea (a crystalline by-product of protein), as well as chloride, sodium, potassium, creatinine (waste from the normal breakdown of muscle), and excess fluid, which exit the body as urine—up to two quarts of it a day. You don’t need both kidneys to function; this redundancy is present in our reproductive organs, too (two ovaries, two testes), a quirk of evolution that acts like an insurance policy against injury. Except strangely, kidneys almost always fail together; the second kidney cannot help us if the other one becomes diseased. And when kidneys fail, the buildup of waste products in the body can be lethal. If catastrophic renal failure (the term for a complete loss of function in both kidneys) occurs, the patient becomes 100 percent dependent upon dialysis, the painful and difficult process of mechanically purifying the blood, for the rest of his or her life. The individual must go to a dialysis center as often as three times a week to have their blood diverted into an external machine to be filtered before being returned to the body. Even with dialysis, many patients, especially in those early days, still died after only a short time. As it goes in the old rhyme, for want of a nail, the kingdom was lost.*
In less than a year, Richard Herrick’s own little kingdom was in terrible shape. He went from a healthy young man to an emaciated patient in the final stages of chronic nephritis, an inflammation of the kidneys that leads to renal failure—and death.With skin the color of bronze, he’d begun experiencing seizures and the onset of psychosis; he was restrained to his bed after biting a nurse. Even dialysis wouldn’t save him for long.
As Richard’s condition grew worse, the doctors transferred him to the Public Health Service Hospital in Brighton, Massachusetts, to be closer to family. His eldest brother, Van, told Richard’s physician, David C. Miller, that he’d do anything to save him, even if it meant giving Richard one of his own kidneys. No, Miller began to assure him, it would only be rejected—except Miller stopped midsentence. He stood silent for a moment as an idea clicked into place. They couldn’t use Van’s kidney, no, but they could use a kidney from Richard’s other brother, Ronald; the two men were identical twins. With Richard’s kidneys literally on life support, Miller gave the order to transfer him to Peter Bent Brigham Hospital. He also called ahead to mention that Richard, unlike most unlucky patients, had a suitable donor.
“It was the perfect human setup for our laboratory model,” Murray would say in later interviews. But should a team of surgeons put one healthy man at risk to save the life of another, even if it were his brother? And what gave Murray the right to decide?
*For want of a nail the shoe was lost.
For want of a shoe the horse was lost.
For want of a horse the rider was lost.
For want of a rider the battle was lost.
For want of a battle the kingdom was lost.
And all for the want of a horseshoe nail.
_______________________________________________
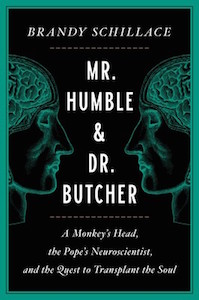
Excerpt adapted from Mr. Humble & Dr. Butcher: A Monkey’s Head, the Pope’s Neuroscientists, and the Quest to Transplant the Soul by Brandy Schillace. Used with the permission of the publisher, Simon & Schuster. Copyright © 2021 by Brandy Schillace.
Brandy Schillace
Brandy Schillace is a historian of medicine and the critically acclaimed author of Death’s Summer Coat: What Death and Dying Teach Us About Life, Living and Clockwork Futures: The Science of Steampunk, and