What Mysteries and Medicine Have in Common
Surgeon and Writer Arnold van de Laar on the Doctor as Detective
How do you decide what is wrong with a patient? In other words, make a diagnosis? Throughout the history of medicine, doctors have tried to answer that question. From the very beginning, they have always been confronted with the patient’s fear. Anyone feeling that their end is nigh, wants to know from the doctor how it will happen. Is there still any hope? How long have I got? Will I suffer pain? To answer these questions sensibly you have to recognize the patient’s problem. Doctors could do that better than anyone, because they had seen more diseases and disorders in their lives than other people. Once they knew what a patient had, they could make a prediction. Those two steps were known as diagnosis and prognosis, medical terms derived from the Greek word gnosis, meaning knowledge. Diagnosis, with the Greek preposition dia (through), means “seeing through” or “insight into.” Prognosis, with the preposition pro (before), thus means a prediction or a prospect.
It was initially sufficient for a diagnosis to describe a disorder, even if you did not really know what was wrong. And you had no need of your hands to do that. If you saw a few pimples here and there, there was probably not much wrong, no matter what it was. But if the patient was covered from head to toe in badly smelling oozing pustules, that was something to be concerned about. In both cases, you could prescribe simple household remedies. If they didn’t help, they also did little harm.
For many centuries, the lack of understanding of the underlying causes of diseases was glossed over with a rather insubstantial story about four alleged bodily fluids, or humors: blood, mucus, yellow bile and black bile. The belief that a disease or complaint arose because the humors were out of balance was not, however, a good starting point for a surgeon. The only way for any of the four fluids to be replenished or reduced in quantity was by bloodletting, and that had very dubious effects. It was a typical remedy of non-surgical doctors.
The next step is not only to recognize and name the problem, but to find out what is causing it. Surgeons want to remove the causes, preferably with a knife. A diagnosis is important for the prognosis, while a cause is important for the treatment. Ileus, for example, is a general term for an obstruction in the passage of food and feces through the intestines. It is a good example of a diagnosis dating from the time before we had any understanding of causes. If there is nothing you can do about it, the prognosis following a diagnosis of ileus is always bleak, no matter what the cause. The patient begins to vomit, is unable to defecate or break wind, develops a swollen abdomen, complains of severe cramps and, if the symptoms do not pass, will die. But if you can do something about it, you need to know not only that it is indeed ileus, but what has caused it. The intestine may be obstructed by a tumor or an inflammation, but also by a chicken bone. The diagnosis remains the same, but the surgical treatment is different in each case. The question asking what is wrong with a patient therefore embraces a number of other questions: what are the patient’s symptoms, what has caused them and how has that led to the disease?
“It was initially sufficient for a diagnosis to describe a disorder, even if you did not really know what was wrong. And you had no need of your hands to do that.”
Because a modern diagnosis entails much more than it used to, the search for the answer has become more and more of a challenge, requiring highly developed skills. Medical doctors and surgeons work in the same way as detectives trying to solve a crime. A doctor trying to find out what is wrong with a patient resembles a detective searching for the perpetrator: identifying the cause of a disease is like looking for the motive for a crime, and establishing how a disease could have developed is reminiscent of following the tracks of the murderer and asking how he used the murder weapon. Just as all real detectives have their own style, doctors also solve mysteries in different ways.
The best writer of detective stories was undoubtedly Agatha Christie and by far the most brilliant character in her books was the detective Hercule Poirot. Poirot is an eloquent man, charming and intelligent, who unerringly solves every mystery that comes his way. But his creator also depicts him as something of an anti-hero. He is polite, but also vain and conceited; objective, but also arrogant and moody; inquisitive, but only willing to help if he finds the case interesting enough, and, though he speaks French, he is Belgian.
The respectable, middle-aged detective is an eccentric, astute and prosperous man with a smartly waxed handlebar mustache, who time and time again—much to the killer’s chagrin, of course—happens to be in the vicinity when a murder takes place. In the Hercule Poirot stories, the plot unfolds according to a fixed formula. Poirot is surrounded by a company of well-defined characters at a more or less self-contained location—a remote country house, the Orient Express stranded somewhere in the snow, or a boat on the Nile. A murder takes place that must have been committed by someone in the group.
As Poirot investigates the murder, it is clear that he knows more than he lets on. In the final chapter, he gathers everyone together in the drawing room or the saloon, to reveal the identity of the killer. He then addresses each of them individually. He explains that each one of them could have committed the murder. Each proves to have a hidden motive and no one has a cast-iron alibi. The butler had the key and access to the knife, the baroness had debts and could therefore make good use of the inheritance, the kitchen maid was jealous—nothing is too outrageous.
After having discussed the motives of each character, however, Poirot presents a counter-argument showing that he or she did not commit the murder. Until he comes to the final one—the killer. But that does not become clear until he has first been through all the others individually. In this way, the tension is built up until Poirot comes to the last remaining character and reveals the circumstances surrounding the horrific murder. His detailed accounts of the potential involvement of each character are so fascinating that we easily forget that the majority of the information he has gathered in fact has nothing to do with the case. After all, only the story about the real killer is relevant to solving the mystery.
This is exactly how an internist works. An internist is a non-surgical doctor, a medical specialist in General Internal Medicine (GIM) who concerns himself with diseases and treats them with medicine. A pulmonologist (who specializes in lung diseases), for example, is an internist, as is a gastroenterologist (digestive system), a cardiologist (heart), a nephrologist (kidneys) and an oncologist (cancer). Internists treat diabetes, cardiovascular diseases, blood diseases, inflammatory diseases, in fact all kinds of diseases, as long as an operation is not required.
Like Hercule Poirot, an internist prefers to solve problems with a list. Poirot starts his analysis with the crime, asking “What happened?” An internist starts with the patient’s complaint and asks “What is the problem?” Then they both isolate the problem and restrict themselves to a well-defined summary of potential culprits. Poirot asks himself which of those present could have committed the murder, while an internist asks himself what might be the possible causes of the complaint. This is known in medicine as drawing up a differential diagnosis. Agatha Christie usually made it easy for Poirot to draw up his list by limiting the number of people at the scene of the crime, but internists too no longer have such a difficult time as formerly in drafting a differential diagnosis. Medicine has advanced so far in the past 50 years that, for most complaints and disorders, it is easy to look up a list of possible causes in a manual, in summary articles, in the medical-scientific literature or on the Internet. An internist thus has a list of differential diagnoses ready in no time.
“A doctor trying to find out what is wrong with a patient resembles a detective searching for the perpetrator: identifying the cause of a disease is like looking for the motive for a crime.”
Then it is time to analyse the evidence and clues. Poirot interrogates and investigates and, if necessary, calls others in to assist. An internist also questions his patient, not only about his current complaint, but also his general state of health, his medical history and family. He examines the patient, requests supplementary tests—blood tests, for example, or X-rays—and will, if necessary, ask the advice of a specialist in another area. Essentially, both Poirot and the internist focus on all potential perpetrators, and not only on the most likely ones.
Lastly, they have to exclude the unlikely culprits. They look closely at each of the candidates to see whether he or she could be guilty. They go through the whole list until there is only one left—the least unlikely. For the detective, it is the main suspect, for an internist, it is referred to as a “working diagnosis.” Exclusion on the basis of probability can lead to very surprising conclusions in the Poirot stories. In Murder on the Orient Express, for example, all those present prove to be guilty, while in Death on the Nile, the victim himself is the guilty party.
Surgeons do not understand this way of working. Their reasoning is usually more pragmatic and linear. Women may come from Venus and men from Mars, but it sometimes seems to surgeons that internists live in a completely different universe, far removed from all earthly logic. A surgeon can, for example, become very hot under the collar when an internist asks him to “exclude ileus” in the case of a patient who no longer displays any symptoms and should actually be discharged, just because the radiologist happened to see what “could be interpreted as a possible ileus” on the CT scan of the patient’s abdomen. For an internist, a result like this upsets his checklist and a suspected ileus must therefore be excluded by a surgeon. For a surgeon, however, that is nonsense. It is immediately clear that he should not operate on a patient with no symptoms simply on the grounds of a suspicion.
Conversely, an internist can be equally irritated by a surgeon who, while operating on a patient with suspected acute appendicitis, discovers that the small intestine is inflamed, rather than the appendix. Inflammation of the small intestine is not treated surgically, but with medicine. Yet the surgeon will stand by his decision to operate, because he found the patient very ill and suspected that he was suffering from life-threatening peritonitis. The internist could present arguments in return that throw doubt on the probability of appendicitis. For example, that the patient had been suffering from diarrhea for a week before the inflammation occurred, which makes the diagnosis less likely.
What lies behind this mutual lack of understanding is a philosophical distinction between deduction and induction, two ways of discovering the truth through logic. Historically, the deductive is older than the inductive method, but both were replaced in the philosophy of science by the scientific method, developed by Karl Popper in 1934.
During the Middle Ages, it was widely believed that human knowledge had already reached its zenith in the golden age of classical antiquity. Doctors and surgeons therefore based their work uncritically on the wisdom of the Greek philosopher Aristotle and the Roman gladiator physician Galen, two men who, with hindsight, did not stand out as providing their theses with a solid foundation in fact. In the Renaissance, scientists once again dared to think critically and drew their own conclusions from general observations. That is deduction. A surgeon knows, as a general observation, that peritonitis can be fatal and that operating to remove the appendix presents a smaller risk. It is then logical, deductively speaking, to conduct an operation in a specific situation in which you suspect the patient may be suffering from appendicitis.
During the Enlightenment, a century later, the experiment developed as a serious basis for science. Conclusions were drawn from specific findings. That is induction. The more indications there are of a certain phenomenon, the more probable it is, and vice versa. A diagnosis of ileus is more probable if a CT scan shows possible indications of the disease, but less probable if the patient displays no symptoms and even less probable if a surgeon sees no reason to operate.
Then Karl Popper introduced the principle of falsifiability and the scientific method. He stated that the truth cannot be discovered. We can only develop a theory of the truth, and then only if we observe one crucial condition: the theory must be formulated in such a way that it can be refuted. This became the basis of all modern medical science. In daily clinical practice, the scientific method works as follows: a clear treatment plan is set in motion for a patient as quickly as possible, based on a working diagnosis. That working diagnosis is based on a falsifiable theory of reality. If the treatment does not have the desired effect, the working diagnosis must be critically reviewed. To reach a working diagnosis, however, induction and deduction remain at the patient’s bedside.
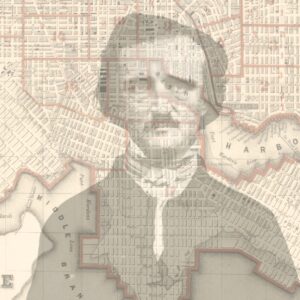
If Hercule Poirot is the master of induction, that other great detective in world literature, Sherlock Holmes, is the master of deduction. Holmes solves his cases in a completely different way, just as a surgeon reaches a working diagnosis differently from an internist. Sherlock Holmes is tall and slim, and stern in appearance. He hardly eats, but smokes all the more for it. He solves mysteries in foggy London, wraithlike and shrouded in secrecy. The basis of his success is the enormous repository of random knowledge in his head. He has studied the meanings of sailors’ tattoos, knows the color and composition of the soil in every part of England by heart, and knows what font is used by each newspaper. These are the general facts on which his deduction is based. The strength of Sherlock Holmes’s method is observation. “The world is full of obvious things which nobody by any chance ever observes,” he says, courtesy of his spiritual father and creator Arthur Conan Doyle—who was also a doctor. He uses deduction to compare what he observes with what he knows. He leaps from observation to observation, moving forward all the time. And, because he does it so well, he rarely has to look at other possibilities or change tack. His method is therefore much more efficient than that of Poirot, more direct, but also more vulnerable as success depends on how well he observes and how much he knows. That is why he works alone. He does have a companion, his friend Dr Watson, but Holmes treats him more as a kind of pupil, from whom he expects little assistance. Watson seems to have been conjured up by Conan Doyle purely to allow the thoughts in the detective’s lonely mind to be translated into a dialogue, so that the reader can also benefit from them.
It is immediately clear that deduction relies entirely on what is in the mind of the detective or the surgeon. By comparison, induction is much more complex, but is also more transparent and objective. Sherlock Holmes could afford not to go into detail about many of his deductions and only explain the whole thing at the end, because his adventures almost always ended in success. Medical specialists, including surgeons, can no longer permit themselves such a luxury. The times when Sherlock Holmes, superior and unfathomable, could outsmart a criminal in the London fog are now over. A modern surgeon no longer presents himself as an individually focused expert who determines the quality of the investigation into a patient’s problem all on his own. Difficult decisions are increasingly made in multidisciplinary consultation, where specialists from various disciplines discuss patients on a case-by-case basis and decisions are thoroughly justified and recorded. The days of deduction are therefore numbered and, who knows, perhaps surgeons and internists will begin to understand each other in the not too distant future?
But one thing will never change. Once a surgeon is standing at the operating table, scalpel at the ready, he is completely alone and everything that he does from that moment, everything that happens to his patient, remains his own, personal responsibility. Then you want to be sure of what you are doing, and you do not help your conscience by working on the basis of probabilities.
__________________________________
From Under the Knife: A History of Surgery in 28 Remarkable Operations. Courtesy of St. Martin’s Press. Copyright © 2018 by Arnold van de Laar.
Arnold van de Laar
Arnold van de Laar is a surgeon in the Slotervaart Hospital in Amsterdam, specializing in laparoscopic surgery. Born in the Dutch town of 's-Hertogenbosch, van de Laar studied medicine at the Belgian University of Leuven before taking his first job as general surgeon on the Caribbean Island of Sint Maarten. He now lives in Amsterdam with his wife and two children where, a true Dutchman, he cycles to work every day. His first book, Under the Knife, is available from St. Martin's Press.