Pig Hearts, Placental Stem Cells, and the Search for the Aging Cure
Chip Walter on the Race for Immortality
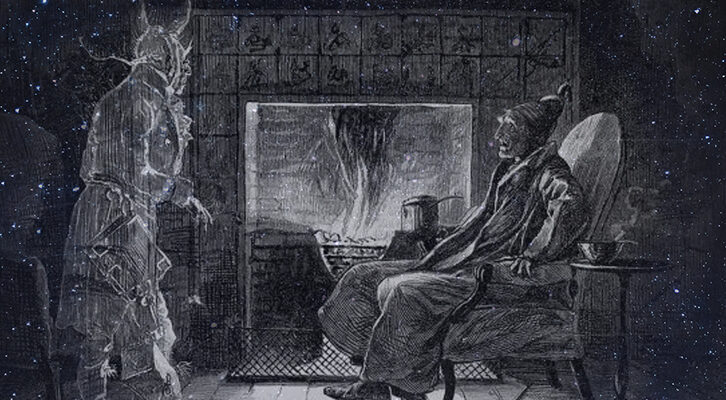
Robert Hariri’s views on human health began to take an unusual turn a little more than 25 years ago, when he was working as a neurosurgeon and trauma doctor at the New York Hospital-Cornell Medical Center. Day after day, he watched patients come into the emergency room with severe brain injuries, and it was a painful thing to witness.
He never forgot the case of a woman who had arrived after a senseless automobile accident. She was young, and the injury was bad. Every time he spoke with the family, the big questions they asked were: “How will she be? Will she come back? Could she be a mother to her children again?” It broke his heart.
Just as the family was asking Hariri these very questions, he was paged for another reason: His wife was being prepped for the first ultrasound of their daughter-to-be. He answered the agonized family as best he could (the prognosis was not promising) and headed to the obstetrics department. But he couldn’t stop thinking about that woman. Doctors, it seemed to him, were getting pretty good at saving people from traumatic injuries, but not doing nearly so well at repairing the resulting damage. There had to be a better way.
As he was thinking about this, Hariri walked into his wife’s room and saw the ultrasound image of his daughter-to-be. Right above the image he could also see the sonogram of her placenta. Compared to the fetus, it was immense, and that made Hariri think.
At the time, the general view of the placenta was that it was nothing more than a system for shuttling blood from the mother to the growing embryo and fetus: a simple vascular interface. But the engineering side of Hariri told him that didn’t make sense. If the placenta was just a vascular interface, it would be small during the early stages of an embryo’s development and then grow pretty much at the same rate the fetus did. But this giant organ was way bigger than the fetus, which meant it had to be supplying a lot more than blood. And that was when the lightbulb lit up.
The placenta wasn’t something that many researchers were eager to scrutinize. Every obstetrician knew that once a baby was born, the organ was immediately disposed of. Doctors called it the “afterbirth.” But Hariri’s explorations revealed that the organ was a very long way from useless. In fact, it provided the very thing an embryo needed to develop into a healthy, living, breathing child: It brimmed with pluripotent stem cells, life’s purest form of cell, capable of morphing into whatever the body required—liver, muscle, even neurons. This was how living things were made as they developed. Some pluripotent stem cells transformed into skin. Others became bones or hearts or kidneys—all the cellular matter that made a human possible. This also made placentas magnificent stem cell factories. Yet every day nearly all of them were tossed in the rubbish!
A discovery like this might have prompted a lot of scientists to write a paper extolling their findings in a peer-reviewed journal; Hariri had done it himself plenty of times. But this time he didn’t write a paper. He wrote a patent. Patent Number 7045148, to be exact, filed in December 2001 and granted the following September. The application explained, in detail, how to collect “embryonic-like stem cells from a placenta” to recharge the stem cells of other humans. The way Hariri saw it, the placenta was a machine, an organic factory designed to create any sort of cell the human body could possibly need, including those that were damaged or dying.
Soon after the patent was created, Hariri founded the Anthrogenesis Corporation and LifeBank, Inc. Later Celgene, a multibillion-dollar pharmaceutical company, bought both companies in 2002, to form Celgene Cellular Therapeutics. Hariri was named chairman, founder, and chief scientific officer.
All that work had gone swimmingly, but by 2012, Hariri felt it was time to more directly explore using placental stem cells to regenerate muscle, bone, and organs, and find new ways to extend life.
*
During the course of his long explorations, Hariri continued to develop some unusual views on aging. He saw three very good reasons to make the affliction go away: It robbed people of their health, mind, and looks. Clearly, the use of the brain and body were pretty useful, but looks? Wasn’t that egotistical, the stuff of Hollywood and those kind of people? No, said Hariri. He held that the older, more frail and haggard people appeared, the more society marginalized them. Aged faces and bodies became a signal for all to see that it was time to move on. So even if your brain and body were strong, if you looked old, you were ushered into the societal dust heap. But what if you had access to medicines created by placental stem cells? Those, at least theoretically, could solve all three problems: regenerating body, mind, and appearance.
If transplants of this kind happen someday, they will essentially transform recipients into chimeras: part pig, part human.This was not an entirely new idea. Before Diamandis and Hariri had begun brainstorming their longevity play with Craig Venter, scientists outside the United States had undertaken stem cell research more aggressively than the FDA in the United States. Among them was the Karolinska Institutet in Stockholm, Sweden, unequivocally regarded as one of Europe’s best medical establishments. At Karolinska, scientists had injected stem cells into patients with blood, brain, eye, bone, and liver disorders, including cancer. The studies were ongoing, but so far the new treatments seemed to be working. Stem cells were simply injected into damaged organs and soon began to regenerate stronger, fresher cells. No petri dishes or complex pharmaceuticals required.
Stem cells were being put to novel uses elsewhere too. In 2016, researchers at another of Venter’s companies, Synthetic Genomics, began collaborating with Martine Rothblatt, founder of United Therapeutics (and before that, creator of Sirius XM Satellite Radio). In one project, the two companies genetically modified the hearts and lungs of pigs. Next, they planned to transplant those organs directly into humans who needed them: something called xenotransplantation.
Pig valves and other assorted porcine organs had been used for decades to bide time for people suffering from failing hearts, but using whole hearts and lungs from pigs creates huge problems because the body rejects them. Venter’s plan was to use genomic sequencers to compare the genomes of pigs and humans, precisely identify the genes that created rejection problems between the two species, use Crispr technology to snip out the offending genes, and then insert the edited versions into pluripotent pigs’ ovaries to create brand-new pigs carrying “humanized” lungs and hearts. It turns out the organs of the average pig are about the same size as the average human, and the genetics are remarkably similar too.
If transplants of this kind happen someday, they will essentially transform recipients into chimeras: part pig, part human. Of course, if the pig’s genes were changed too much, their stem cells might not survive. “It’s not like by changing a couple genes you’ve got it solved,” Venter said. Nevertheless, so far, the experiments had been promising, if not perfect.
But maybe none of this would be necessary if placental cells could perform their magic. Imagine an aging baby boomer whose cells are giving out from all of the damage that his DNA hasn’t been repairing as well as it did back at age 25. Sore knees or, worse, a heart or spine or pancreas or brain starting to sputter.
Now, rather than a heart transplant (pig or otherwise), or great buckets of drugs to keep the body clattering along, doctors could inject Hariri’s placental medicines. As the old stem cells give out, the pristine, new ones step in. Later, when another part of the body begins to run down, a new, fresh batch could be supplied, and so on, until boomers everywhere were being youthfully topped off and their cells reset—not only healthier, but actually younger, and therefore not marginalized! Ken Bloom, HLI’s president, had said himself that stem cells might someday find a way to push the length of human life beyond 120 years—maybe way past that.
But as compelling as placental stem cells might appear, they weren’t perfect. At least, not yet. For one thing, the fresh stem cells that one receives from their own body will always adhere to whatever genetic ailments that body’s DNA already carries. If someone is genetically prone to arthritis or heart problems, or even addictions or depression, those problems are going to reappear eventually. Cancer could also be an issue. Introducing new stem cells into the body of someone with a predisposition to various cancers might actually encourage tumors rather than eliminate them. In some ways, cancer cells were like pluripotent stem cells in that they can replicate indefinitely.
Down the road, Crispr technology might fix problems like these with a couple of nicks of the Crispr scissors. But Crispr had its own problems. It could easily change and swap cells, but once the DNA of a pluripotent stem cell is rearranged, that change remains forever and is even passed along to the next generation, just as if evolution and your own parents had provided the DNA. One would want to be very careful that there were no unintended consequences when swapping these genes.
*
Already the impossible had happened in 2018, when the scientific world learned that Chinese scientist He Jiankui had used Crispr to alter embryos that were then implanted in a woman who later bore twin girls. He did this entirely on his own. His goal, he said, was to eliminate genes that could cause the newborns to get HIV, because the children’s father was HIV-positive. But the fact that the scientist had independently and forever changed the DNA of living humans appalled scientists and bioethicists. If one gene like this could be edited, what would stop rogue scientists from creating someone’s idea of a superbaby? Or unwittingly developing a baby with a new and unknown disease?
The fear was that this kind of gene editing was moving too fast. Scientists were still trying to suss out the ways stem cells reacted to the different bone or liver or heart cells they might replace. How long were they effective? Which cells triggered what signals? These explorations took time, and they were complicated. It wasn’t like changing a carburetor. And of course, there was the problem of the Big Black Box, the brain, which, for reasons only evolution could fathom, did not generate large reservoirs of stem cells like many other parts of the anatomy.
As one scientist put it, “The science will go where the science will go.”And what if older neurons were replaced wholesale with new stem cells? They might scramble different sectors of the brain by destroying the new connections between the originals. Fiddle with those, and who knew what mayhem might follow? Memories, learning, and other cerebral functions that the brain had grown accustomed to might simply vanish. On the other hand, in the case of a disease like Alzheimer’s, maybe new memories would be better than no memories at all.
One age-related affliction particularly intrigued Hariri, and he suspected curing it could slow death’s march pretty quickly: sarcopenia. Sarcopenia was a disease that accelerated the loss of muscle in some people before their time. Since the FDA defined it as a disease, clinical trials were possible. Furthermore, anyone who was aging—and that was everyone—suffered from a form of sarcopenia. It was simply what happened as time passed. Hariri had found that by the time the average Homo sapiens turns 25, muscle mass begins to drop off at the rate of 1 to 2 percent a year. By age 60, half of it is gone.
One might think that this loss would only affect a body’s strength and steadiness, and that would be true. But there are other factors as well. It turns out that most of the blood in the body resides in muscle. Its high venous capacitance is essential to long-term health, because venous capacitance is what delivers the goods to your immune system. So now a 60-year-old human hasn’t only lost half of his muscle mass, but also half of his venous capacity and immune system. This means that anyone over 25 has begun suffering from a chronic form of sarcopenia—and though you can slow the process with proper diet and exercise, it inevitably continues. There’s no way around it. In Hariri’s mind, placental stem cells offered a perfect cure, because the cells could regenerate muscle. That would, in turn, reduce fat, renovate the vascular and immune systems, and generally reverse aging. One 2009 study even disclosed that increasing muscle lowered the likelihood of cancer.
Would a world brimming with baby boomers find a treatment for sarcopenia appealing? Forget worrying about ageism or flabby arms, compromised immune systems, or the sad smiles of people as they gazed at the elderly couple over there with their walkers, thinking, Aw, isn’t that sweet? Because that couple, even with lots of years in the bank, would not need walkers anymore. They would be vigorous, healthy, upright, and perfectly capable of pulling their weight in the real world. One hundred could become the new 60! That, at least, was how Hariri and Diamandis saw it playing out.
But right now, all of that was still science fiction. No one was going to be biologically “topped off” with stem cells and rejuvenated just yet. Nevertheless, Hariri and Diamandis—the two Celularity founders—had high hopes. The company was already developing several clinical trials to move as quickly as possible toward FDA approval. Maybe stem cells would become the holy grail of radical longevity, and thousand-year life spans would abide as the human race broke its evolutionary bonds. Who could say? All you could do was try. As one scientist put it, “The science will go where the science will go.”
__________________________________
Excerpted from the book Immortality, Inc.Copyright © 2020 The Human Light and Power Co., Inc. and William J. Walter, Jr. All rights reserved. Reprinted by arrangement with National Geographic Partners. Available January 2020 wherever books are sold.
Previous Article
Marcelo Hernandez Castillo:A Journey to the Home of My Ancestors