On the Persistence of Magical Thinking in the Face of Grief
Mary-Frances O’Connor Considers the Mutually Exclusive Truths Our Grieving Brains Can Hold
A few years ago, an older colleague of mine passed away. I spent some time with his widow in the months afterward. As a prominent sleep researcher, her husband had traveled quite often to attend academic conferences. Over dinner one night, she shook her head as she told me it just did not feel like he was gone. It felt as though he was just away on another trip and would walk through their door again at any minute.
We hear this kind of statement quite often from those who are grieving. People who say this are not delusional; they simultaneously are able to explain that they know the truth. They are not too emotionally frightened to accept the reality of the loss, nor are they in denial. Another famous example of this belief comes from Joan Didion’s book The Year of Magical Thinking. Didion explains that she was unable to give away her deceased husband’s shoes, because “he might need them again.” Why would we believe that our loved ones will return, if we know that’s not true? We can find answers to this paradox in the neural systems of our brain, systems that produce different aspects of knowledge and deliver them to our consciousness.
If a person we love is missing, then our brain assumes they are far away and will be found later. The idea that the person is simply no longer in this dimensional world, that there are no here, now, and close dimensions, is not logical. The question to consider is, Why do we believe we will find them?
*
If we take seriously what bereaved people tell us, then it seems the brain can persist in two mutually exclusive beliefs. On the one hand, we have the clear knowledge that a loved one has died, and on the other, the simultaneous magical belief that they will return. When a loved one has died, we have a memory of learning that they died. This memory might be of the phone call informing you that your brother died, etched in your mind with lots of detail—where you were in the dining room, what you were cooking, how hot it was in the room, the smell of onions. These are what we call episodic memories; they are detailed memories of a specific event.
If a person we love is missing, then our brain assumes they are far away and will be found later.
Perhaps your memory of the death occurred because you were there when it happened. When my father passed away in the summer of 2015, my sister and a dear family friend and I had been taking turns sleeping in the room with him in the hospital he had chosen for hospice care. On that particular night, I had said good night to him, although he was not responding to us anymore. I got a few hours of sleep on the little couch in the room. In the middle of the night, I woke up filled with a sense of awe, a frequent experience in those last few days (along with feelings of utter exhaustion and lack of confidence that I could go on any longer). I checked on my dad, and then I decided to go for a walk outside, moved by a similar sense of awe I feel when looking at the marvelous stars in the rural Montana night sky. If you’ve ever been far, far away from city lights, you know that there are so many stars, the night sky looks like it is scattered with glittering sand. I walked the circular path around the hospital, designed to give staff and visitors a place to stretch their legs.
I went back to the room, and Dad was still breathing very, very slowly. It was truly amazing, I thought, that his life could be sustained with so little breath. I went back to sleep. In the wee hours of the morning, a nurse leaned over me, hand on my shoulder. “I think he’s gone now,” she said. I went to my dad’s bedside. He was so peaceful, so little, looking both like an infant and an old man at the same time. He looked exactly the same as a few hours before, except that his breaths had gone from very, very slow to none at all.
My experience of my father’s death was extremely peaceful and filled with awe, and I was comforted by loved ones and caring professionals around me. I was able to really focus on what was happening at the time, and as I look back on it I usually feel quite peaceful, even if very sad. I count myself extraordinarily lucky, because I got to experience what could only be called a good death. It was aided by the fact that he was in a hospice program, designed by the people who know the most about creating conditions most likely to lead to a good death. Many deaths are not at all like this. People experience fear, terror, pain, helplessness, or extreme anger at the moment of their loved one’s passing, especially if it occurs in violent or terrifying circumstances, in accidents or emergency rooms.
During the COVID-19 pandemic, many people were unable to be with their loved ones when they were admitted to the hospital and were not at their bedside when they died. Without the opportunity for saying good-bye, for expressing love, gratitude, or forgiveness, and without the memory of seeing our loved one’s physical decline and death, ambiguity may surround the “realness” of the death. Research shows that ambiguous loss, such as when family members are disappeared by a political regime or missing and presumed dead from an airplane crash or in wartime conflict, complicates the grieving process. One reason may be that part of our brain is wired to believe that our loved one is never really gone, and without the overwhelming evidence from our memories of their decline or death, rewiring our understanding may take longer or cause greater distress.
____________________________________________________
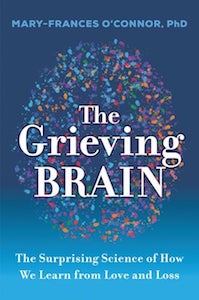
Adapted from THE GRIEVING BRAIN by Mary-Frances O’Connor and reprinted with permission from HarperOne, an imprint of HarperCollins Publishers. Copyright 2022.
Mary-Frances O'Connor
Mary-Frances O’Connor, PhD is an associate professor of psychology at the University of Arizona, where she directs the Grief, Loss and Social Stress (GLASS) Lab, investigating the effects of grief on the brain and the body. O’Connor earned a PhD in clinical psychology from the University of Arizona in 2004, and completed a post-doctoral fellowship in psychoneuroimmunology at the UCLA Semel Institute for Neuroscience and Human Behavior. Following a faculty appointment at UCLA Cousins Center for Psychoneuroimmunology, she returned to the University of Arizona in 2012. Having grown up in Montana, she now lives in sunny Tucson, Arizona.