Meghan O’Rourke on the Self-Dissolving Difficulty of Chronic Illness
Searching for the Self Amid Pain
One of the hardest things about being ill with a poorly understood disease is that most people find what you’re going through incomprehensible—if they even believe you are going through it. In your loneliness, your preoccupation with an enduring new reality, you want to be understood in a way that you can’t be. “Pain is always new to the sufferer, but loses its originality for those around him,” Alphonse Daudet observes in In the Land of Pain. “Everyone will get used to it except me.”
Worrying that your symptoms are psychosomatic—or even imagined—is part of life for many people with poorly understood illnesses. Although the experience of illness is not just in the head, it is also not just in the body. The person enduring such an illness faces a difficult balancing act. On the one hand, she must advocate for herself, even when doctors are indifferent or ignorant, and not be deterred when she knows something is wrong. On the other, she also must be willing to ask whether an obsessive attention to symptoms is going to lead to better health. The patient has to hold in mind two contradictory modes, in other words: insistence on the reality of the disease and resistance to her own catastrophic fears. I found it hard, in the fall and winter of 2012, to strike that balance. I was increasingly worried.
After all, a terrible anxiety attends chronic illness. Over time, it becomes difficult to untangle the suffering from symptoms like pain from the suffering inflicted by the anxiety over the possibility of more pain, and worse outcomes, in the future. This does not mean that the illness is in the mind; rather, the mind—that machine for making meaning—makes endless meanings of its new state, which may themselves influence the experience.
It was in this recursive hall of mirrors, trying to adjust to my body’s ailments, that I lived.
There is a loneliness to illness, a child’s desire to be pitied and seen. But it is precisely this recognition that is elusive. How can you explain and identify your condition if no one has any grasp of what it is you suffer from and the symptoms wax and wane? How do you describe a disease that’s not always there?
The hardest thing to convey to doctors or friends was the debilitating fatigue, which many other patients I knew experienced as well. Complaining of fatigue sounds like moral weakness; in New York City, tired is normal. But the fatigue of physical dysfunction, I came to recognize, is as different from normal sleep deprivation as COVID-19 is from the common cold. It was not caused by needing sleep, I thought, but by my body’s cellular conviction that it needed to conserve energy in order to fix whatever was wrong. The feeling erased my will, the sense of identity that drives most of us. The worst part of my fatigue was the loss of an intact sense of self.
I experienced a mounting anxiety: everything was wrong, and that wrongness was inside me, but I wasn’t sure anymore who that “me” was.
It wasn’t just that I suffered brain fog; it wasn’t just the loss of self that sociologists talk about in connection with chronic illness, in which everything you know about yourself disappears and you have to build a different life. Rather, as I got sicker that winter, I no longer had the sense that I was a distinct person. On most days, I felt like a mechanism that moved arduously through the world simply trying to complete its tasks. Sitting upright at my father’s birthday dinner at a quiet restaurant required a huge act of will. Normally, absorption in a task—an immersive flow—can lead you to forget that you feel pain, but my fatigue made such a state impossible. I might, at the nadir of my illness, have been able to write any one of these sentences, but I would not have been able to make paragraphs of them.
To be sick in this way is to have the unpleasant feeling that you are impersonating yourself. When you’re sick, the act of living is more act than living. Healthy people have the luxury of forgetting that their existence depends on a cascade of precise cellular interactions. Not you. “Farewell me, cherished me, now so hazy, so indistinct,” Daudet writes—a line I now often thought of.
My mental sensation of no longer being a person had a correlating physical symptom: my eyes no longer seemed like lenses onto the world. They seemed, rather, to be distinct parts of my body, as perceptible as fingers—oddly distant, protuberant, like old-fashioned spectacles. My face was a mask I was conscious of at all times. It made me feel categorically fraudulent. I could feel the fat in my cheeks and the weight of my bones as I spoke. I experienced a mounting anxiety: everything was wrong, and that wrongness was inside me, but I wasn’t sure anymore who that “me” was, or how to express what was happening.
I was thirty-six when I realized that not everyone in their twenties and thirties was in pain all the time.
As Virginia Woolf testified in On Being Ill, “English, which can express the thoughts of Hamlet and the tragedy of Lear, has no words for the shiver and the headache … The merest schoolgirl, when she falls in love, has Shakespeare or Keats to speak her mind for her; but let a sufferer try to describe a pain in his head to a doctor and language at once runs dry.”
For me the hardest part was not being comprehended, or not believed. “Physical pain does not simply resist language but actively destroys it,” writes Elaine Scarry in The Body in Pain. “To have pain is to have certainty; to hear about pain is to have doubt.” The same was true of all my symptoms, none of which could be seen.
In those months I was lonely in a way I never had been before. I could taste the solitude of the human body like brine in my mouth, a taste that never left me.
I was 36 when I realized that not everyone in their twenties and thirties was in pain all the time. I had been in pain of one sort or another since college, much of it muscular or joint pain, some of it gynecological. In 2011, I started having serious hip pain and was diagnosed with a torn labrum and arthritis, for which I had surgery that I was slow to recover from. By 2012, when I came to understand I was sick, pain was only one of my symptoms, and not even the worst. But its constancy was wearing. It moved around my body, changing from day to day, worse one day in my hips, the next my neck or my right thumb. My muscles were always tight; shooting pains ran from my shoulder to my neck, or down my legs.
Some days, the pain tipped from manageable to consuming, as if my brain had been caught in an unexpected electrical storm. When it did, it was as if a high-pitched noise no one else could hear was in the room. It distracted me and made me irritable. I was both present with others and off in my head, attending to the pain, trying to gauge its neural contours. One day, pulling down a box of sweaters from a high shelf, I felt pain radiate through my neck and back, which froze up. X-rays found that I had cervical spine scoliosis, compression of a cervical disc (likely the cause of my acute pain), and extensive arthritis in my neck; the doctor, who knew about my hip, mused that I was having a lot of issues with my connective tissue.
I started physical therapy, where I had to rank my pain level on a scale of 1 to 10 week after week, an exercise I found impossible: How to describe intermittent severe pain on the same scale as constant middle-range pain, which I found more debilitating? Attempting to reduce pain that was context dependent to a number just made it clear that there was no way to make this invisible symptom legible to others. And the poet in me found all the metaphors for pain to be limited. “Burning,” “tingling,” “stabbing”—these words did little to describe pain’s reality, which ebbed and flowed according to its own logic. Pain was an empire of its own, well defended against language’s forays against it.
At the urging of first one friend, then another, I read everything I could by John Sarno, a New York physician who had written several best-selling books about his conviction that a great deal of back, neck, shoulder, and carpal tunnel pain is caused by repressed negative emotions—such as stress, anger, and anxiety—in people inclined to bottle things up. He argued that these repressed emotions can cause muscle pain by reducing blood flow to the area in question, leading to a syndrome he termed “tension myositis syndrome” (TMS).
Sarno, who died in 2017, believed that if such patients acknowledge and exorcise their negative emotions, their pain will disappear, because it is the body’s way of distracting the mind from a trauma or source of anguish. Open to anything, I did what he advised, wondering if in fact I suffered from repressed anger. Could it be that something like my ongoing grief at my mother’s death was the real problem?
But none of Sarno’s exercises worked for me—though I went so far as to see a therapist trained in his methods. I grew frustrated that so many people wanted to assume that my pain was emotional in origin without knowing anything about my medical history. The idea that emotional tension could lead to pain struck me as logical based on my limited understanding of biology, but it also seemed to me that some people embraced Sarno’s framework as yet another way of finding certainty where uncertainty lived. Usually, it became clear that Sarno’s approach had been a magic solution for them. (It had worked for them; therefore it must work for you—a mindset one encounters a lot.) I suspected that something more complicated was going on, and that I was not yet done with uncertainty.
All I knew was that day after day the pain moved around. I did my best to ignore it.
*
My father, who was just emerging from a period of acute mourning for my mother, lived in a small town in Connecticut, about ninety minutes from Brooklyn, where my parents had moved in 2003 so that my mother could become the head of a local private school. My father ran the languages department there. Jim and I saw him periodically for dinner, sometimes with my brothers, Liam and Eamon, who also lived in Brooklyn. I told him that I wasn’t feeling well, but in the absence of an identifiable illness, what was he supposed to say or do? “I’m sorry you’re feeling so bad,” he once said to me on the phone, in his indirect Irish American way, apropos of nothing. Today, I hear the empathy and helplessness he must have felt, but at the time the concern felt remote.
In my fatigue and pain I couldn’t find the words to make myself legible to others.
I was beginning to confront the fact that the Hashimoto’s diagnosis, though crucial, did not explain my ongoing poor health. As my doctor had noted enthusiastically at a recent visit, the lab work showed my autoantibodies were still almost nonexistent. The thyroid medication had normalized my hormone levels. I should be feeling well. Neither she nor any other doctor was able to give a name to my ongoing illlness; it was invisible, vague. My brothers were sympathetic but busy with their own lives, still wrestling with the aftermath of our mother’s death. It was shocking to me how much I missed her, how much worse it was to be sick without her comfort and counsel. At times I thought I would slowly slip away unseen and no one would notice because the shell of my body was still there.
One night I went to a work event in the West Village, at which people I hadn’t seen for months were dressed in party clothes—sheen of silk, bare shoulders, men in leather shoes—smoking on the balcony. “How are you feeling, Meghan?” a tall poet asked, putting his hand on my shoulder in genuine concern, a cigarette dangling between his lips. “Meghan!” cried two others I hadn’t seen in a year, leaning languorously against the balcony wall in a way that made me nervous. What was there to say? It was New York City; everybody was striving to feel more, be more. I had the sensation that I needed to find a better story to tell about my condition, because of course I had no story at all. In her poignant memoir A Body, Undone, about a bike accident that left her largely paralyzed, the scholar Christina Crosby writes, “Whenever you offer an account of yourself to others, you labor to present yourself as coherent and worthy of recognition and attention, as I am doing right now.”
This labor was precisely what I was failing to perform; in my fatigue and pain I couldn’t find the words to make myself legible to others. (And I still have not found them. This text is full of silences and vagueness and lacunae: when I write “brain fog,” I imagine that your mind slides over the idea, unless you, too, have suffered from it.) In the absence of that recognition, I began to see myself as not only incoherent but also unworthy, ashamed that I craved comfort from others.
I chatted on the balcony, sorrow growing in me, then went inside and got my coat to go home.
*
In this period, I did find comfort in books. In bits and pieces, I was reading poetry I loved, and trying to write poems, too. I managed to write a few short essays I was proud of. But it was often almost impossible to read. Usually, I fell asleep trying, the light from my bedside lamp warm on my left cheek, the dark purple walls of our tiny Brooklyn bedroom cocooning me as buses roared past, taking people to and from their jobs.
In those late fall months, I lived as if in a locked room. I could only look out the windows, catching fragmentary glimpses of life as I’d once enjoyed it, growing even more determined to find answers.
Outside, my friends were meeting in the park, eating picnic lunches in sweaters as their children poked one another with sticks, or hailing taxis in a sudden downpour, giving the stranger at a party a second, hungry look.
Inside, it was dark and stuffy, and I labored to survive an illness no one could see. In this way the undiagnosed suffer, doubly alone.
At times I thought the only way to escape was to become mad, like the narrator of Charlotte Perkins Gilman’s “The Yellow Wall-paper,” who goes slowly insane when her husband, a physician, treats her case of “a slight hysterical tendency” (brought on by the birth of her son) by keeping her locked in a room on the top floor of a house they have leased.
I would have to make a window in my experience through which I could climb out, whatever that meant.
Why does a diagnosis matter so much to you? a friend asked me at one point.
I know many people who are suspicious of diagnoses—they think of them as labels that reduce or stigmatize. I knew, already, that a diagnosis was not going to answer all my questions. But I craved a diagnosis because it is a form of understanding.
Knowledge brings the hope of treatment or cure. And even if there is no cure, a diagnosis is a form of knowing (the word “diagnosis” derives from the Greek gignōskein, “to know”) that allows others to recognize our experience and enables us to tell its story. I felt acutely the absence of a story I could tell others. Without a story, who—or what—would help me get better?
Alice James, William and Henry’s sister, was sick from adolescence on with a disease no one could exactly name or treat (though she was diagnosed with hysteria). Near the end of her life, when she was finally given a breast cancer diagnosis, she rejoiced in her diary, “To him who waits, all things come! . . . Ever since I have been ill, I have longed and longed for some palpable disease, no matter how conventionally dreadful a label it might have.” Anyone who has suffered from an unnamed illness can understand the perversity of the logic. At last, James writes, she was released from “the monstrous mass of subjective sensations,” which “that ‘medical man’ had no higher inspiration than to assure me I was personally responsible for, washing his hands of me with graceful complacency.” She died of breast cancer within a year of the diagnosis. So challenging was living with an unidentified illness that she welcomed the terrible news with what sounds like excitement.
When I read this in her diary, on a brisk October night, I set the book down. The night’s shadows had lengthened, the streetlamps with their sodium glow brightened the darkness beyond. I couldn’t pinpoint what was disturbing me, except that it had to do with the waste of this life and this mind.
Sitting on my couch, I felt Alice James’s shadow inside me. I knew what it felt like to have your illness go unnamed. I could imagine what it was like to give up, to feel your mind go as wobbly as your body, reconciling yourself to the idea that death would really be a relief—a respite from lonely suffering. I could sense, inside my body, the muddled pains of hers.
It was also all too easy for me to imagine how the 19th-century conception of hysteria led her to assume that her symptoms were her own personal failings. I felt a wasteland of sorrow. Too much of my own life had been spent wondering if what was wrong with me was a deficiency of character. I also felt fear: Would my doctors assume, as her doctors had of Alice, that some mental strife was the source of my disease—a dis-ease, in other words?
This was why I wanted others to see what was happening to me, to know that I was locked away in the room alone. If they knew, perhaps someone could find a way to get me out. Instead, I feared, I would be relegated to a world of the imaginary ill, exiled to an invisible kingdom from which I would never be allowed passage.
My testimony wasn’t doing the job. (“You look great.”)
Yet I felt deeply that something was wrong. I can’t put this into clinical language. All I can say is that it was a bone-deep, a cell-deep conviction: that whatever was wrong was not in my head. The symptoms—roving neurological pain, headaches, flu-like aches, sensitivity to food—were too specific. And my lab work had so many small clues. Low vitamin D. Anemia. The many viruses.
Where was the scientist, the doctor, who felt acutely “how liddle he knows” and would come to help me, to help all of us in this condition?
I knew such doctors were out there, and at night I prayed for them to succeed.
Please, I thought, know that we are here and we need your help.
__________________________________
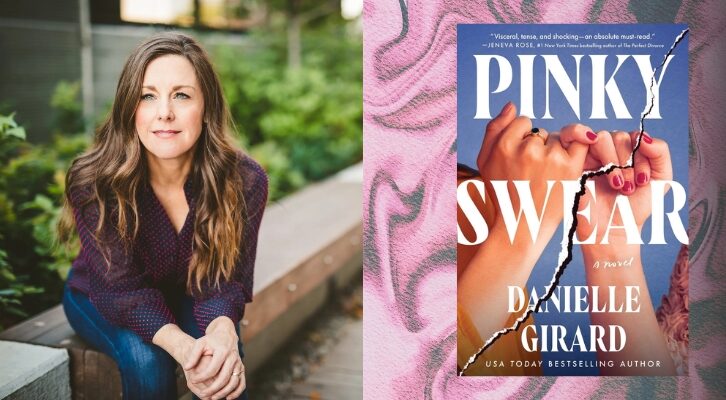
From THE INVISIBLE KINGDOM: Reimagining Chronic Illness by Meghan O’Rourke published on March 1, 2022 by Riverhead, an imprint of Penguin Publishing Group, a division of Penguin Random House LLC. Copyright © 2022 Meghan O’Rourke.
Meghan O'Rourke
Meghan O'Rourke is the author of the collections Halflife and Once, and a memoir, The Long Goodbye. A former editor at The New Yorker, she has served as culture editor and literary critic for Slate as well as poetry editor for the Paris Review. Her poems and essays have appeared in The New Yorker, The Best American Poetry, the New Republic, and Poetry, among others. The recipient of a Guggenheim Fellowship, a Radcliffe Fellowship, and other awards, she lives in Brooklyn.