Inside the Emergency Room on the Eve of the COVID-19 Pandemic
Farzon A. Nahvi on the Early Days of a Public Health Disaster in the Making
What follows is a series of text messages between a group of ER physicians across the country.
*
February 28, 2020
LA: So, crazy coronavirus story to get everyone worked up. Family of four presented with fever and cough after just returning from South Korea where a close family member they had contact with is hospitalized for coronavirus. Any guesses what the CDC recommended?
DE: My guess is no testing?
SE: I don’t think I want to know.
KB: New guidelines say test
LA: Haha yea no testing
WS: Yes. They don’t want to test anyone.
We have so many of those at my shop
Every time [we call the department of health] they say don’t test.
BX: Best way you can say you don’t have cases is by not looking for them.
*
March 2, 2020
WS: [REDACTED] hospital has a Covid case
KB: A second Manhattan case?
WS: I think it’s the first [test confirmed case]
SE: It’s crazy to think NYC and LA aren’t already full of it.
It’s just that nobody is testing.
*
March 5, 2020
ES: [REDACTED] hospital has one now [too]
KB: Has anyone tested for community spread? NYC Dept of Health only tests for known contacts or travel risk now.
QS: Yea, [we] haven’t tested for community yet
BX: Seems dumb when you’re potentially more likely to be exposed to it in NYC at this point
ES: That’s my favorite part
HO: Astronaut applications on usajobs.gov open tomorrow for anyone interested in escaping Earth.
*
March 11, 2020
ES: It’s starting here
About to intubate for respiratory failure. Bilateral interstitial pneumonia. Hypoxic failure.
It’s going to be a dumpster fire when there are multiple
WS: ES that’s almost certainly it. It’s all over. [REDACTED] hospital, [REDACTED], [REDACTED], my hospital
ES: Yeah
KB: Just intubated a confirmed corona.
My plan as of now is if you fail nasal cannula and need a nonrebreather you are likely to progress rapidly and I’m going to get ready to tube you
DE: Same
WS: Seems better to just rapidly intubate. It’s source control. Of course, we will run out of vents and ICU beds but…
KB: That’s my practice until we run out of vents
*
March 20, 2020
KB: Just got off a phone call with our ventilator rationing committee.
QS: I just followed up on everyone I’ve admitted (and all age ranges and all without respiratory distress at time of admission but with other factors, whether it was hypoxia, or how bad chest X‑ray was, or age etc.) and like 90% of them are now intubated
JJ: Wow that’s insane—all Covid positive?
QS: Ya. And that’s just my patients. I was just chart checking the ICU/Step Down Unit patients and similar story for most of them
WH: Miss you all…just got out of a crazy shift…everyone is pretty much positive now
KB: We aren’t liberating any of our vented patients
*
“We aren’t liberating any of our vented patients,” my friend had written in his text message. His language was revealing. One does not require liberation from a savior, of course, but from an oppressor. And so, while the country was celebrating healthcare workers as heroes, we knew that the truth of our circumstance was much more complex.
We did what we could to save our patients from their disease, and then, later, we would do what we could to liberate them from those very efforts.
We were scrambling to take action despite having no clear idea of what the right course of action was. We prescribed medications and performed interventions while wondering aloud whether they would do any good. Our lack of information did not preclude our mandate to act. And so, at best, our efforts were a paradox: we did what we could to save our patients from their disease, and then, later, we would do what we could to liberate them from those very efforts.
This is not unusual. As much as we may prefer a narrative where the right course of action is clear and where what is helpful shares no border with what may cause harm, such a narrative has never reflected the reality of my experience. An honest narrative is never a clean one. Like so many things in our lives, there was no playbook and no perfect solution. We existed, as we often do, within a series of impossible circumstances.
Reality is subtle, grayscale, and nuanced. It is playing the role of both savior and oppressor at the same time. It is taking action while recognizing that action to be imperfect, and moving forward despite being unable to see clearly what lies ahead.
Life, in short, is complicated.
I cleared my messages and put my phone back in my pocket. I had just biked home from my shift in the emergency room, but the fog of anxiety that permeated the hospital in the spring of 2020 had followed me. To regain a sense of ease, I would first have to carefully decontaminate myself and my belongings. Whether on the front of my mask, the sides of my shoes, or on the strands of my unkempt hair, I had no doubt that I had brought the virus home with me.
I had already developed my routine, but had not yet become so habituated to it that I could perform it mindlessly. Like a student driver, I had to remain conscious of the manner and sequence of my motions. During the Ebola crisis, it was this step—the removal of our protective gear—that was the most important.
It was here that healthcare workers were most likely to become infected with the Ebola virus. If used properly, the equipment worked: it was human error that was most often our downfall. Mindless scratches of the nose and careless removals of facemasks had set off morbid cascades from which some never recovered.
This fact struck me as a strange irony. After working a long day in an intense, high-stakes environment, it might have been when we exhaled and relaxed that we were most at risk. The lifesaving intubations, the adrenaline-pumping atmosphere of a crashing patient, the anxious moments when we held our breath as we made sure our patients could breathe—these were the points at which things certainly felt most dire.
Yet it was possible that it was only when everything died down—when the danger was neither palpable nor visible—that we were actually most vulnerable. The mundane act of removing one’s mask was imbued with the potential of a slow-motion suicide. It would be the equivalent of successfully flying a treacherous combat mission behind enemy lines in a thunderstorm, only to crash the plane upon landing it back home on a calm and sunny day. An anticlimactic end, but one that was just as real and permanent as any other.
Still, there were limits to what we could learn from our experience with Ebola. Our current environment was very unlike our environment then. The Manhattan hospital I worked in during the Ebola crisis was designated as New York City’s Ebola receiving center—we saw numerous patients thought to have the virus, and one who actually did. Wearing our normal attire through most of the day, we would pause to don our personal protective equipment only as we prepared to see a patient suspected of having the disease.
Afterward, we would be received by a “doffing coach,” whose entire role consisted of guiding us through the meticulous removal of our protective gear. This step of carefully removing our soiled equipment was so critical that experts did not trust us physicians to do it correctly on our own. During the Covid crisis, there was no institution designated a coronavirus receiving hospital, as every hospital had already become one by default. There was no role for a doffing coach since our workday never contained a moment free enough from the threat of Covid to actually remove our protective equipment.
And so, I never did. Long after my shift had ended, I found myself riding my bicycle through the streets of Manhattan with my hospital facemask still fixed securely to my face, its metal clips continuing to dig into the bridge of my nose until I would arrive home to finally remove it.
We existed, as we often do, within a series of impossible circumstances.
I entered my building and climbed the stairs to my apartment, carrying my bicycle on my shoulder. While I would normally ride the elevator, I recently began to avoid it upon returning from shift. My building included plenty of elderly tenants—neighbors whose smiles I knew well but whose names I could not produce despite years of sharing the same hallways.
Through time and habituation alone, I had developed a special affection for the silver-haired lady with the wobbly blue walker, the mumbling man whose wardrobe consisted exclusively of camo and cutoff denim, and the wrinkly lady whose small talk consisted of “beautiful day, huh?” no matter the weather. Despite our exchanging little more than nods and pleasantries, these individuals had become deeply woven into the fabric of my life. It was with concern for them that I began my new routine.
My father chuckled when he learned that I was carrying my bicycle up four flights of stairs. “It’s about time the donkey enjoyed some payback from his jockey,” he said laughing. I rolled my eyes but secretly admired his perennially carefree and upbeat attitude.
He was raised with no electricity or running water and had witnessed several of his siblings die from the usual maladies of growing up poor in a developing country. I had always wondered whether my father had developed his cheerful outlook toward life despite the hardships he experienced, or, perhaps, precisely because of them.
As the pandemic began to roar, the death count in the emergency room climbed, and friends and family started to fall ill, I realized that I would finally put this theory to the test. Would the current tragedy make me more like my father, or less?
__________________________________
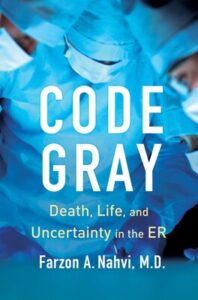
Excerpted from Code Gray: Death, Life, and Uncertainty in the ER by Farzon A. Nahvi. Copyright © 2023. Available from Simon & Schuster.
Farzon A. Nahvi
Farzon A. Nahvi is an ER physician at Concord Hospital in Concord, New Hampshire, and a clinical assistant professor of emergency medicine at the Geisel School of Medicine at Dartmouth. Prior to this, he worked as an ER physician and clinical assistant professor of emergency medicine at the Mount Sinai Health System, NYU Langone Health, NYC Health + Hospitals/Bellevue, and the Manhattan VA. He is a graduate of Cornell University and NYU Grossman School of Medicine. He has written for the New York Times, The Washington Post, The Guardian, Daily News (New York), New York magazine, and other publications. In April 2019, he testified as an expert witness before Congress in the nation’s first Medicare for All hearing.