How Stress Creeps Through Social Inequity to Shorten Lives
Dr. Arline T. Geronimus on Stress and the Human Biological Canvas
Stress is a strangely diffuse concept that everybody thinks they understand. The word stress is used loosely to cover a broad array of feelings, perceptions, circumstances, and physiological reactions. What any one of us deems stressful is influenced by our individual personalities and life histories, and is also partially a matter of how the social groups we are part of define stress.
For example, the stress of juggling the demands and deadlines of one’s professional job—whether an accountant or a zoologist—with the needs and expectations of one’s children is qualitatively different from the stress of being a soldier on a battlefield. But upper-middle-class working parents who perform that juggling act every day identify their constellation of personal and professional responsibilities as stressful, and they understand one another when they call this “stress.”
The stress of being “crazy busy” like those parents, within the context of having many options and resources, is also different from the stress experienced by parents working multiple minimum-wage jobs while battling with their landlords to fix the heat in their apartments and sending their children off to underresourced, physically toxic school environments. And it is different from the stress a bereaved Erica Garner described experiencing as she felt compelled to take on the mantle of a leader in the struggle to end police brutality.
How much of a toll such experiences of stress take on the body, both in the short and long term, and how they cause weathering, is the focus here. But this chronic physiological stress is very different from stress in the age-washing perspective, which views it as something largely within our control, if only we learn how to handle it.
Part of the age-washing narrative is about stress. We are told that the key to a long life is not just to make the right lifestyle choices—to eat well, move more, and get a good night’s sleep—but to stress less, and have a positive attitude. In a 2013 article on a site called the Guardian Liberty Voice, a reporter presented the statistical findings that stress in a woman’s thirties is associated with Alzheimer’s disease in her later years. So the prescription for avoiding Alzheimer’s, she writes, is to “place your demons in a box, embrace your midlife crisis with a smile and high heels, and try to make amends with stress, for the less he visits you, the better.”
Challenges, setbacks, and tragedies may be nonnegotiable parts of life, we are told, but how we face them is within our control. “The toll stress takes, research has shown, depends on how it is viewed,” says the issue of Time magazine with the potentially 142-year-old baby on the cover. “The 70‐year-old will always be 10 years older than the 60‐year-old. But if you’re talking about how many years both of those people have remaining, put your money on a happy, active 70 over a cynical, sedentary 60.”
Based on this description, we would certainly put our money on Kate’s longevity. Yet, how representative is she of the baby boom cohort? My research shows that many baby boomers died or became disabled by age 50. They didn’t get to experience old age, let alone redefine it.
So how well would Kate’s decision to “worry less,” and the Guardian Liberty Voice’s advice to put your demons in a box, smile, and make amends with stress, serve Beverly, a Black woman living in a Yonkers, New York, housing project who has experienced lifelong poverty and long bouts of unemployment? A New York Times Magazine article that profiled her as she, too, was approaching 50, paints quite a different picture of what middle age looks like.
According to journalist Helen Epstein, Beverly had asthma, diabetes, high blood pressure, rheumatoid arthritis, gout and an enlarged heart, and her blood has a dangerous tendency to clot spontaneously. She is 48, and she had her first heart attack in her late 20s. One of her brothers died of heart failure at 50, and another died of kidney failure at 45, as did a sister who was 35. A young cousin recently died of cancer. In the past three years, at least 11 young people she knows have died, most of them not from gunshot wounds or drug overdoses, but from disease.
Do we really believe a positive attitude or the decision to become more adventurous and learn West African dance would cure—or prevent—what ails Beverly? Being sick with such a litany of ailments is not unusual for low-income Black women. In a nationwide analysis, my colleagues and I found that 60 percent of all working- and reproductive-age Black American women suffer four or more stress-mediated chronic diseases by age 50.
The idea of living to age 95 or 100 must seem mythical to these women.
In her ethnographic study on welfare, children, and poor families in three cities, the sociologist Linda Burton found that 60 percent of the primary caregivers in the study suffered multiple morbidities, despite the fact that the vast majority of them were younger than 39 years old.
For example, Barbara, age 37, suffered from a range of chronic health conditions that included diabetes, back injuries, kidney problems, high cholesterol, migraines, hernias, depression, and anxiety. Thirty-two-year-old Amanda had Sjögren’s syndrome (an autoimmune disease), severe dental and gum disease, arthritis, acid reflux, and hypertension. Francine, age 30, had stomach cancer. Even 23-year-old Hazel had gastric ulcers, asthma, liver disease, emphysema, dental and gum disease, and diverticulitis, and was clinically depressed.
The mothers of many of these women were sick enough to require care. Many of the grandmothers had already died by their early fifties of cardiovascular disease, strokes, or cancer. This was an additional source of distress for their adult daughters as well as a window into their own futures.
One 19-year-old who lived in the same Yonkers neighborhood as Beverly reportedly lost so many loved ones to disease and accidents that whenever she thought about it, she was stricken with panic. “My heart beats so fast, and I can’t breathe, and there’s just death going through my mind the whole time.”
And in the three-cities study, Burton and colleagues found that in the most distressing of circumstances, cycles began to appear between parent and child, in which the chronic conditions of one exacerbated the conditions of the other. Fiona, whose 10-year-old son was diagnosed with depression, said: “He’s depressed and worried about my problems and I feel guilty that he has taken my problems to heart.”
The idea of living to age 95 or 100 must seem mythical to these women; and their male counterparts have even shorter life expectancies, on average. Not that there are no “old old” (over age 85) people in the communities I’ve studied, whether in Central Harlem, Eastside Detroit, the South Side of Chicago, or the Watts area of Los Angeles—they’re just comparatively rare.
So which children in high-poverty urban or rural areas can expect to make it to age 85, 95, or even 100? My research shows that prior to the pandemic a 16-year-old Black girl in Eastside Detroit had a 29 percent chance of living to age 85; for a boy in the same circumstances, the likelihood dropped to 9 percent. For whites in high-poverty areas of Detroit, the odds were nearly as bad, with 30 percent of girls and 12 percent of boys likely to make it to 85. Poor whites in Appalachian Kentucky fared a bit better than their urban counterparts, with 36 percent of girls and 16 percent of boys expected to live to 85, but these figures are still far below nationwide averages.
For kids in any of these areas, even reaching retirement age—65—is an achievement. In Watts at the dawn of the twenty-first century, fewer than one out of two 16-year-old Black boys and two out of three 16-year-old Black girls could expect to survive through middle age. To put this into perspective: The average national odds of reaching age 65 are four out of five for 16-year-old boys and eight out of nine for sixteen-year-old girls.
If these grim statistics conjure up tabloid images of homicide deaths or drug overdoses, think again. Almost 50 percent of all early deaths among Black residents of the South Side of Chicago could be attributed to circulatory disease or cancer. Only 6 percent of early deaths among women and 14 percent among men were lost to homicide. That said, homicide is a significant cause of death for Black males aged 15 to 24 on Chicago’s South Side. But, importantly, the largest disparities in mortality between white and Black people, and between the poor and nonpoor, occur not among youth, but among those ages 25 through 65.
Weathering is a universally human physiological process. It just occurs more to members of oppressed and exploited social identity groups.
We also found that Black residents of disinvested high-poverty neighborhoods who did survive to middle or old age—poor and middle-class alike—were more likely to have health-induced disabilities than white individuals across the nation who survived to the same ages. In fact, the differences between these groups in terms of healthy life expectancy—defined as the number of years of life lived without any health-induced disabilities—were huge. In one study, we found that 28 years of healthy life expectancy separated Black teenage boys living in high-poverty areas from white teenage girls living in more affluent areas.
Among Black people in high-poverty areas of Chicago, the proportion of people who were likely to survive to age 50 without a health-induced disability was only 50 percent. For whites in Appalachian Kentucky, the proportion was similarly small. As some of these statistics show, weathering is not all Black versus white.
While I focus on specific racialized populations in this book—Black Americans in particular—it is essential we remember that weathering is a universally human physiological process. It just occurs more to members of oppressed and exploited social identity groups, who are often subjected to severe conditions of material hardship, toxic environments, social and cultural disruption, mis‐recognition, or erasure, and need to engage in high-effort coping to survive day‐to‐day.
Indeed, since the 1990s, life expectancy has stagnated among the least-educated white Americans while continuing to grow to varying degrees for other groups, including low-socioeconomic-status whites in other Western nations. The most widely publicized interpretation of excess deaths among less-educated US white people is an increase in opioid overdoses, a cause that allows the age-washed perspective to consider their deaths preventable exceptions.
But, horrific as the scourge of opioids has been, it is not the main cause of premature death in less-educated white people—just as homicide and drug overdoses are not the main cause of premature death in the inner city, despite what the tabloids would have us believe.
Excess deaths of poor and working-class whites occur, in the main, as a result of chronic circulatory disease and cancer—diseases that are mediated by our stress response. And I don’t mean the kind of response where we meet the stresses of our daily life with a smile and a deep breathing routine, but rather physiological stress responses that are activated automatically.
Stress in the context of weathering refers to underlying and automatic biological processes that respond to lived experience. In the right measure and circumstances, these processes are protective and health-promoting. But when such responses are excessive and prolonged, they can cause damage. And since these physiological stress responses are indeed automatic, set in motion spontaneously by our bodies in response to various stimuli, they are not under our conscious control.
The inner workings of our bodies are always active and adapting, physiologically responding as necessary to changes in our environment. The late Rockefeller University neurobiologist Bruce McEwen referred to these adaptive processes as allostasis; they help us to maintain stability, or homeostasis, the tendency of the body to seek and maintain balance within its internal environment, even when faced with an external challenge.
Some external challenges are quite mundane, such as retaining our balance when we move from a seated to a standing position. Another example: our bodies physiologically work to maintain a temperature of 98.6 degrees Fahrenheit (37 degrees Celsius) by sweating in hot environments and shivering in cold ones. We don’t decide to sweat or shiver; our hypothalamus, which we can think of as the hormone control panel of the brain, automatically activates the processes that heat and cool the body. That our bodies have this automatic capacity to calibrate our biological processes to respond to our environmental contingencies is a wondrous fact.
For the most part, our ability to quickly react to stressors and maintain homeostasis is health-protective. Your muscles precisely contract and relax in order to keep you balanced as you rise to your feet, thanks to quick signals between the cerebellum and vestibular system in your brain. You shiver long enough to get to your well-heated home, where someone awaits you with a hot cup of cocoa. You sweat long enough to get yourself to an air-conditioned movie theater.
Even a massive stress response to a life‐or‐death threat is designed to be short. Seeing a cheetah in the savanna or a Big Bad Wolf in the forest triggers a release of hormones from the sympathetic nervous system, which in turn stimulates the adrenal glands, which release adrenaline and other hormones that activate increases in heart rate, blood pressure, and breathing rate.
The result of all these actions is that oxygenated blood circulates to your large muscles quickly, preparing you to fight or flee. After the threat is gone, the body quickly returns to its pre-arousal levels. As the Stanford neurobiologist Robert Sapolsky so graphically puts it: “If you are a normal mammal, what stress is about is three minutes of screaming terror on the savanna, after which either it’s over with or you’re over with.”
During those three minutes, your body mounts an automatic response without your having to decide consciously that it was necessary. If mammals had to make a conscious decision about how to react to every threat, we would have gone extinct long ago. In the context of meeting a cheetah on the savanna, this reaction works well; much better, presumably, than stopping to dazzle it with your smile and high heels, or taking a moment to meditate, feel gratitude, or cognitively reframe the situation. There’s no time for cognitive reframing. The cheetah is there and it wants to kill you. Your cognitive capacities have been turned down spontaneously in favor of your affective ones. If you’ve ever had a sudden brush with death— say, a car barreling toward you while you’re crossing the street—you’ve had some experience with this automatic physiological response.
__________________________________
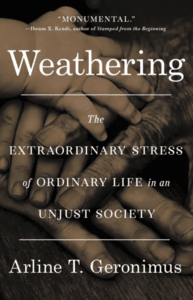
Excerpted from the book Weathering by Dr. Arline T. Geronimus. Copyright © 2023. Available from Little, Brown Spark, an imprint of Hachette Book Group, Inc. All rights reserved.
Arline T. Geronimus
Arline T. Geronimus is a Professor in the School of Public Health and Research Professor in the Institute for Social Research at the University of Michigan, where she also is affiliated with the Center for Research on Ethnicity, Culture, and Health. She is an elected member of the Institute of Medicine of the National Academies of Science.