How Social Medicine Can Help Us Understand Pandemics
Paul Farmer on the Interplay of a Virus and Its Environment
“An understanding of the definition of a pathogen is not required when a clinician is faced with an infected patient who needs treatment. However, if we are to understand disease-associated microbes and discover effective therapies, we will also need to appreciate their fundamental biology and the ecological setting in which they secure a niche . . . So-called emerging infectious diseases reflect various aspects of imbalance in the relationships between host, pathogen, and environment. Many of the most serious and feared infectious diseases occur when humans are infected by microorganisms that prefer, and are better adapted to, another mammalian host. In fact, most emerging infectious diseases in humans are of zoonotic origin.”
–David Relman and Stanley Falkow, “A Molecular Perspective of Microbial Pathogenicity,” in Principles and Practice of Infectious Diseases, 2010
“Le microbe n’est rien, le terrain est tout.”
[“The germ is nothing, the land is everything.”]
Louis Pasteur, September 28, 1895
*
Ebola was first identified in October 1976, in a mission hospital in the village of Yambuku, in the northern reaches of Zaire, which today is known as the Democratic Republic of the Congo. But there’s no reason to believe that the pathogen was new to the clinical desert. It took time for the virus to be recognized as a novel species, a process that required staff, stuff, space, and systems.
This process of discovery began after blood samples from infected patients were collected in Kinshasa, the capital of Zaire, some seven hundred miles from Yambuku. Some were sent thousands of miles away, to Antwerp, Belgium, where, with the help of an electron microscope, they were classified as “a Marburg-like virus.” Other samples were dispatched to the U.S. Centers for Disease Control and Prevention, in Atlanta, and to the Army High Security Laboratory in Porton Down, England. Soon the virus would be declared a new member of the filovirus family, along with Marburg, and given the name Ebola, after a river that runs close to Yambuku. By the time that happened, however, the virus had already killed many of those seeking and giving care in or around the village.
One of several people credited with the discovery of Ebola is Peter Piot, a Belgian infectious-disease doctor who was among those dispatched from Antwerp to Yambuku to conduct an investigation of the outbreak, which claimed the lives of several Flemish nuns. Piot was a junior partner in the investigation, especially after the arrival of seasoned smallpox hands and other heavies from the Centers for Disease Control, but he did speak Flemish. He has since worked, over a forty-five-year career, in places as varied (and connected) as Kinshasa, Antwerp, London, and Geneva. From the early days of his training, Piot loved the work of microbe hunting and its therapeutic promise. As he has written in his memoir, “You came in and figured out what the problem was. And if you managed to figure it out quickly enough—before the patient died, basically—then you could almost always solve it, because, just like my medical school professor of social medicine had said, solutions had by this time been found for almost every kind of infectious illness.”
For clinical practitioners of social medicine, the problem beyond scientific discovery—whether of microbes or vaccines or therapies—was one of delivery. How do you deliver solutions old and new to those in greatest need? Under colonial rule, at least across much of Africa, the question was rarely posed and never answered. While “extractive science”—evaluating afflicted villagers and then shipping samples to labs in Europe—may uncover previously unknown pathogens and lead to the discovery of new therapies, these will be offered mostly to those who are deemed more worthy than others. This was a problem that had bedeviled even the most well-meaning colonial health officers, regardless of their empires of origin. It had bedeviled even missionaries, including Flemish ones laboring in their former colony. Medical historians working in the social-medicine tradition have shown as much in study after study.
If nothing else, Ebola teaches us the importance of social medicine, which focuses attention not only on why plagues afflict some and spare others but also on how inevitable mutations—social and biological, among pathogen and host—are related to differential risks for infection and death. As Peter Piot and all who ventured from cities like Antwerp to villages like Yambuku discovered, if you want to address the delivery problem, you need a social medicine incorporating staff, stuff, space, and systems. But West Africa, like the northern Congo, has not known this sort of social medicine, because of a series of extractive arrangements—slavery, racism, colonialism, and war. Its medical and public-health systems have failed repeatedly to deliver on the promise of discovery.
*
Social medicine includes the study of how pathogens—and pathogenic forces—get in the body, how they take their toll, and how and why these processes vary so radically from time to time, place to place, and person to person. Practitioners of social medicine pay attention to pathogenesis, which medical dictionaries define as “the development of morbid conditions or of disease; more specifically, the cellular events and reactions and other pathologic mechanisms occurring in the development of disease.” By any criterion, more has been learned about the pathogenesis of serious Ebola infections in the past few years than in all of the years since 1976.
If nothing else, Ebola teaches us the importance of social medicine, which focuses attention not only on why plagues afflict some and spare others but also on how inevitable mutations are related to differential risks for infection and death.
That’s not saying much. Ebola, like Marburg, has received scant attention from the best basic scientists and clinical researchers, and from the world’s largest research-based pharmaceutical concerns, for a simple reason: there’s not much money in it. Valiant exceptions aside, few well-equipped researchers have focused on how these viruses cause human disease, and even fewer have focused on treating it by taking up the clinical battle against the pathogens. If social medicine is a field suggesting that clinical endeavors should be informed by context—looking around (at what’s going on outside the hospital) and looking back (in time)—then the social medicine of filoviruses is nascent at best.
The West African Ebola epidemic made this clear. There was more focus on looking around (at the mistrustful locals) than at looking back (at the events and processes that made them so mistrustful). Disturbingly, what we’ve learned in its aftermath is that some of our post-2013 discoveries about these viruses are better termed rediscoveries—or, in harsher terms, a failure to recall lessons from the not-so-distant past, including those learned and forgotten in towns and villages from the Sudan to Angola, and in European cities like Marburg, Frankfurt, and Belgrade. But unforeseen developments can lead to rapid and positive change.
There’s been stunning progress, for example, in our understanding of the structures of these viruses. Molecular biology and phylogenetics have permitted not only the publication of Ebola’s genome but also the construction of its family tree, with many of its ramifying branches limned by large teams of laboratory scientists and computational geneticists, including Humarr Khan and Pardis Sabeti and their colleagues. This achievement did not come to pass because of some long-standing and exceptional focus on a pathogen afflicting primarily the rural poor in Africa, although that’s what motivated Sabeti et al. The achievement occurred in part because much research on lethal viruses has been propelled by fear-based funding.
Nor was this scientific achievement linked to robust efforts to match it with clinical ones. The desire to identify “the molecular basis of human disease”—the name, or something like it, of one of the massive textbooks I tried to digest in medical school more than thirty years ago—is above reproach. We all live in bodies, composed of tissues and organs and fluids; these components of our bodies in turn are made up of cells, they of molecules, and molecules of atoms. And we all, alas, become diseased or injured, or both, on the way to a universally shared destination.
Infectious-disease clinicians (mostly doctors and nurses) recognize typical and atypical presentations of disease caused by viruses that sicken humans; they’re usually also informed about other matters relevant to clinical practice. It’s a lot to know, since that practice requires familiarity with a host of diagnostic tests of varied accuracy; specific therapies (antiviral drugs, for example) and some notion of how they are best dosed and for how long; their complications and side effects; nonspecific therapies (such as fluid resuscitation, correction of acid-base imbalances, and replenishment of lost electrolytes, as well as therapies to counter symptoms ranging from diarrhea to vomiting); common complications of viral infections (for example, the secondary or opportunistic infections seen in the course of afflictions ranging from influenza to measles, as well as HIV); and late complications of viral infections capable of persistence among human hosts who survive acute infection.
Social medicine includes the study of how pathogens—and pathogenic forces—get in the body, how they take their toll, and how and why these processes vary so radically from time to time, place to place, and person to person.
Clinicians and public-health practitioners alike also learn about preventive measures, including vaccines, postexposure prophylaxis (for rabies, say, or HIV), and respiratory or contact precautions (such as barrier nursing and infection control) needed to prevent a pathogen’s spread within crowded settings such as hospitals, nursing homes, and schools. (For those working in the sorts of places described in these chapters, “crowded settings” include mines, military barracks, prisons, refugee camps, and a host of informal settlements and precarious slums.) But there’s a lot that even the most seasoned clinicians don’t know, much of which, embarrassingly enough, is termed “basic science.”
Most clinicians, including nurses and doctors who treat viral diseases on a daily basis, will admit that the basic science of virology and immunology is wondrously and devastatingly complex. We know that these pathogens are classed as either DNA viruses—herpes viruses, for example—or RNA viruses, like measles, coronaviruses, and filoviruses. We learn that mutations can confer increased virulence, as the influenza pandemic of 1918 suggested even before the causative pathogen was identified, or increased resistance to proven therapies. But the clinical and epidemiological implications of specific mutations are usually contested or unclear.
The same might be said of the basics of viral pathogenesis, even though they are easy enough to master. In the straightforward reviews read by medical students and trainees in infectious disease, there’s usually mention of seven steps in the interaction between virus and host: entry into the host (in this case, us); primary replication in infected cells; spread within the host; “tropism,” or preference, for specific host cells or tissues, such as liver, lungs, or brain; secondary replication in these preferred tissues and cells; cell injury and death; and the host’s immune response in tandem with the clearance or persistence of virus. These steps have been studied—during the course of acute illness, through autopsies, and after experimental infection of living animals—for many years.
Some of these seven steps are also studied in laboratory models using human or animal cells and tissues. In the case of the filoviruses, our familiarity with the unfolding of viral pathogenesis has been limited by more than a lack of adequate funding: Ebola and Marburg are classed as pathogens to be studied only in biosafety-level-four, or BSL-4, laboratories. Few such labs exist. (One proposed for Boston was approved, funded, and built only to see its opening delayed for years because of objections from frightened neighbors.) Since the discovery of Ebola, much filovirus research has relied on studies using primates. The course of Ebola caused by the Zaire species is thought to be fairly similar in humans and rhesus macaques, the most common unwilling volunteer. So, too, with Marburg.
But not all steps in filovirus pathogenesis are readily studied in animal models—even in the right labs and even when the intent is to develop specific therapies and vaccines. It’s too dangerous. During the West African outbreak, researchers like Pardis Sabeti, who lacked ready access to BSL-4 laboratories, were obliged to develop “fake viruses” in order to study Ebola mutations.
To understand the complexities of real-world epidemics, you need a firm grasp of social medicine.
__________________________________
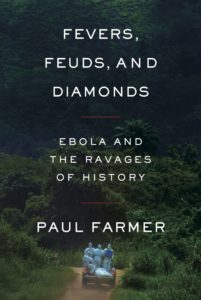
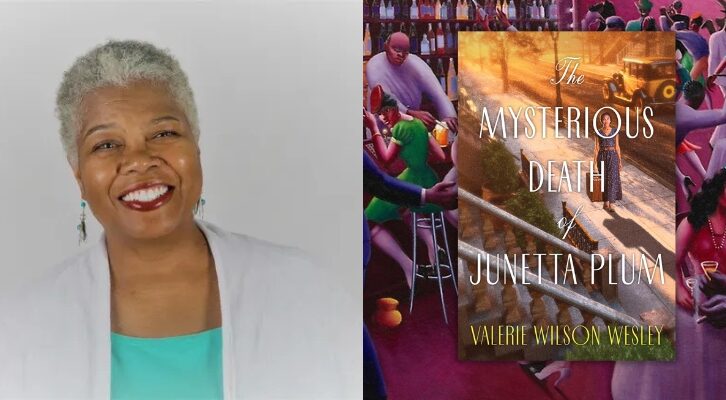
From Fevers, Feuds, and Diamonds: Ebola and the Ravages of History by Paul Farmer. Used with the permission of Farrar, Straus and Giroux. Copyright © 2020 by Paul Farmer.
Paul Farmer
Paul Farmer is the Kolokotrones University Professor and Chair of Global Health and Social Medicine at Harvard Medical School as well as chief of the Division of Global Health Equity at Boston's Brigham and Women's Hospital, and a founding director of Partners In Health. Among his numerous awards and honors is the Public Welfare Medal from the National Academy of Sciences.