How Did Shakespeare Kill (And Heal) His Characters?
Kathryn Harkup on the Many Ways To Live and Die on the Elizabethan Stage
“I know when one is dead, and when one lives.”
King Lear, Act 5, Scene 3
*Article continues after advertisement
Shakespeare’s plays are full of characters dying, both onstage and offstage. There are discussions about death too, and threats to kill. Loss of life in the tragedies and histories is expected, but death lurks in the comedies too, where plays that are usually associated with laughter and romance also have characters who are threatened with execution (Comedy of Errors, Measure for Measure) or appear onstage in mourning (Twelfth Night). In Love’s Labour’s Lost, a play full of frivolity and witty word play, the announcement of a death brings the comedy to a juddering halt.
Advances in medicine have extended our average stay on earth considerably when compared to those living in Shakespeare’s day, but death is still inescapable. No matter how much we may try to prolong or cheat the inevitable, “All that lives must die, / Passing through nature to eternity” (Hamlet). The manner of our death, however, is likely to be very different from the experiences of our predecessors in the 16th century.
Today our final moments will most probably be spent in a hospital or care home where medically trained staff are close at hand. Sixteenth-century London had only three hospitals: St Bartholomew’s, St Thomas’s and Bethlem hospital for the insane. These institutions were strictly for the poor and few of those who entered expected to leave. Pistol’s beloved Doll is the only one of Shakespeare’s characters to go to a “’spital,” where we are told she died of the “Malady of France” (syphilis). Her death comes in the same play, Henry V, as the demise of Shakespeare’s great comic creation, Falstaff, but his death is the more typical experience of the day as he dies in a domestic setting surrounded by friends.
Few of those living during this time could have escaped witnessing death at close quarters.
In the 16th century, and for some considerable time afterwards, births and deaths usually occurred in the home surrounded by friends, family and local gossips, rather than by the professional medical support expected today. Only the most shameful of illnesses such as syphilis, or contagious diseases such as plague, kept visitors away. Few of those living during this time could have escaped witnessing death at close quarters.
Death itself was considered natural, with the exception of murder, suicide and witchcraft. But dying suddenly, alone or in disreputable circumstances was considered a bad death. This is not to say that the Elizabethans were complacent about dying and did nothing to avoid it. Medical treatments of various kinds were administered, wounds were treated by surgeons and attempts were made to revive the apparently deceased, as is shown in Shakespeare’s plays.
There are hundreds of medical references in [Shakespeare’s] work, direct and oblique, showing an understanding of health and anatomy far beyond that of any other playwright of his day.
The complexity of the human body means there are many points of vulnerability that can potentially bring about our end. Most of the time our bodies carry on doing their complex essential tasks without us really paying them much attention. But we are quick to notice when those processes aren’t working properly, and seek medical help to make us feel better and prevent things becoming serious, or even fatal. The Elizabethans were no different in being preoccupied with their health and seeking medical help. The form of help they received, however, was very different.
There were many options for consultations open to patients in Shakespeare’s day, but choice was governed by a patient’s ability to pay rather than medical expertise. Options ranged from the highly regarded, university educated and very expensive physicians, to the much cheaper choice of the nearest wise woman. However, the size of the fee and education of the practitioner didn’t improve the chances of recovery. The harm done by common forms of treatment generally outweighed any benefits linked with expertise or price.
The Elizabethans were no different in being preoccupied with their health and seeking medical help. The form of help they received, however, was very different.
In the 16th century and beyond, women were central to medical treatment and shouldered the bulk of the health-care burden. The range of female medical providers ran from friends and relatives offering basic nursing, to wise women who offered cures and treatments, and midwives who assisted at births. The skills of midwives were certainly highly regarded, and no pregnant woman would have considered having a male practitioner attend the birth other than under the most extreme circumstances. Despite this, midwives were certainly at the bottom of the professional medical hierarchy.
At the top were licensed physicians, called doctors because they had been educated at Oxford or Cambridge. Physicians learned from Latin texts, made diagnoses, treated internal ailments and prescribed medicines, but they did not cut into the body. Anything requiring a knife and involving bleeding was left to surgeons, found on the next rung down of the medical hierarchy.
Surgeons not only bled their patients, a common medical treatment of the day; they also performed minor surgery such as removing stones, amputations, trepanning (drilling into the skull) and stitching up wounds. Barber-surgeons cut hair as well as flesh, hence the traditional sign outside barber shops of a red and white striped pole, signifying the blood and bandages of their profession. At a similar level of respectability were apothecaries who made and sold remedies, and may have carried out some unofficial diagnosing.
There was little concept of disease as a distinct entity. For example, fever was seen as an illness in itself, rather than a symptom exhibited by many different diseases.
As well as medical people with accepted professional status, right at the bottom of the pile were all manner of unlicensed healers. Quackery was rife, but the lack of a license did not necessarily mean the individual was a quack. Many cheap, and sometimes effective, treatments might be offered by women and men who had no official training, but vast experience.
All of these various types of medical practitioner are depicted, or at least mentioned, in Shakespeare’s plays. Apothecaries appear on stage to sell poisons; surgeons are sent for to treat the wounded after altercations with swords; wise women are consulted; and doctors are depicted, both real and fictional. Shakespeare went further than all of his contemporaries in his portrayal of medicine and use of medical terms in his plays. There are hundreds of medical references in his work, direct and oblique, showing an understanding of health and anatomy far beyond that of any other playwright of his day.
One example of Shakespeare’s in-depth medical knowledge was his apparent references to the theory of the circulation of the blood. This discovery is usually attributed to William Harvey and was first described by him in a lecture he gave in 1616 (although Harvey didn’t publish his theory until 1628, after the playwright’s death). However, the theory was certainly known before 1616 by a few medical men in mainland Europe and is hinted at in several Shakespeare plays, decades before it was accepted by the English medical establishment. Lines such as, “You are my true and honourable wife; / As dear to me as are those ruddy drops / That visit my sad heart” (Julius Caesar) and “The tide of blood in me / Hath proudly flow’d in vanity till now” (Henry IV, Part II) certainly suggest an appreciation of blood flowing, even if Shakespeare didn’t explicitly state that blood flows in a continuous circuit.
People did not expect healers and medicine to cure them and they certainly didn’t think that taking medicine would make them feel better.
Where Shakespeare gained his knowledge has been speculated over for centuries. Some have suggested that he must have known William Harvey personally to gain insight into his theories. There is, however, no proof that they were acquainted. There were no compendium-style medical textbooks to study, but there were a lot of written treatises on specific ailments and medical theories that he could consult. Questioning medical practitioners directly might have been another route. Aside from personal experience of consulting medical practitioners for himself and his family, one doctor Shakespeare certainly did know was Dr John Hall, who married his daughter, Susanna, in 1607. The medical information contained within his plays certainly became more detailed after their wedding.
Shakespeare often poked fun at medical practices, the state of medical knowledge and the dire remedies that were doled out, but he held the doctors themselves in high esteem, with one notable exception. Dr Caius in The Merry Wives of Windsor, a pompous, self-important man much ridiculed by those around him, may be based on Dr Theodore de Mayerne, a prominent French physician who treated several French and English sovereigns. De Mayerne was president of the College of Physicians and apparently appeared very scholarly and sure of himself; perhaps he was a figure ripe for having a little fun made at his expense.
Notable among Shakespeare’s collection of doctors, quacks and apothecaries is the (fictitious) female practitioner, Helena, in All’s Well That Ends Well, who successfully treats the King of France after all other male physicians have failed. Indeed, the doctors made him worse. Her medical knowledge is said to come from her physician father, Gerard of Narbon. Women were officially barred from studying medicine but knowledge was often shared through correspondence between practitioners and women. The character and the story of All’s Well That Ends Well are not original to Shakespeare, who adapted the tale from Boccaccio’s Decameron. Both versions illustrate how many women were respected for their medical knowledge, gained through informal methods of learning and sharing information, as well as personal experience of treating the sick.
Women are portrayed in all the usual medical roles that might be expected of them in Shakespeare’s day. Though they don’t appear on stage, wise women are mentioned in both Twelfth Night and The Merry Wives of Windsor. Twelfth Night, and several other plays, also includes one of the more curious methods used for diagnosing disease and prognosticating over the fate of 16th-century patients—uroscopy. Flasks of a patient’s urine would be collected and sent off to a doctor or wise woman for inspection, just as Falstaff does in Part II of Henry IV:
Falstaff: Sirrah, you giant, what says the doctor to my water?
Page: He said, sir, the water itself was a good healthy water, but, for the party that owed it, he might have more diseases than he knew for.
The upper echelons of the medical hierarchy turned their nose up at uroscopy but it continued to be popular. Examining the color, clarity and odor of urine was supposed to offer clues to the state of the patient’s health and temperament. Elaborate color-wheels of shades of urine were produced to assist diagnoses. As Speed says in Two Gentlemen of Verona, “these follies are within you and shine through you like the water in an urinal, that not an eye that sees you but is a physician to comment on your malady.”
In reality, only the most crude assumptions could be made by this type of examination and uroscopy certainly didn’t deserve the trust many placed in it. Blood in the urine obviously indicates a serious problem with the kidneys, a sweet taste would be caused by diabetes and blue or dark urine can be a sign of porphyria or other diseases, but it is far from an exact science. Testing urine today can reveal vital information about a patient’s health but this was simply not possible before the advent of modern analytical techniques.
Instead, the College of Physicians recommended measuring the pulse and judging fever by feeling the patient’s forehead with the back of the hand, neither of which were terribly effective without stethoscopes and thermometers. All a physician really had at his disposal was his knowledge and observation through visual inspection, smell, taste and listening to the patient’s complaints.
Until germ theory was developed in the 19th century, medical practitioners were left guessing as to the cause of many diseases and therefore had little hope of treating them.
After diagnosis a treatment would be recommended to the patient and could differ greatly depending on which school of medical thought the doctor subscribed to. There were two theories of medicine battling to save lives in the 16th century. There was the traditional Galenic system of humors: good health was enjoyed by those who had the correct balance of four humors—black bile, yellow bile, phlegm and blood. An imbalance of humors brought on illness and so physicians tried to restore the equilibrium through recommending special diets, blistering, sweating, purging (vomiting and excreting) and bleeding. The system of humors was more or less abandoned by the late 17th century, even though patients continued to be bled long after that. But traces of it can still be found in modern English; we still talk of good and bad humors to describe a person’s temperament. Such phrases would have had a more literal significance in Shakespeare’s day.
The alternative approach to health competing for attention in the 16th century was a new theory from Paracelsus (a Swiss physician almost exactly contemporaneous with Shakespeare), based on observations and a belief that everything was due to chemical processes (though his chemistry was very different from the modern science). He pioneered the use of synthetic chemicals and minerals as medicines.
Shakespeare was well aware of both theories and satirized the competition between the two in All’s Well That Ends Well, “Why, ’tis the rarest argument of wonder that hath shot out in our latter times.” But, with a few notable exceptions, such as laudanum, there was little medical benefit in any of the treatments on offer at the time, and some of them threatened considerable harm to the patient. As Timon of Athens puts it to a thief, “Trust not the physician; / His antidotes are poison, and he slays more than you rob.”
In spite of their best efforts, before the beginning of the 18th century, medical professionals had little impact on the population they treated.
Helena’s treatment for the King in All’s Well That Ends Well claims to be completely harmless and promises to cure the King’s fistula (an abscess in the chest) within two days. This benign remedy, whatever it might have been, and its rapid and complete success, is in stark contrast to the medical treatments available at the time. Regardless of whether the Galenic or Paracelsian system was used, treatment was for symptoms and not the underlying disease. There was little concept of disease as a distinct entity. For example, fever was seen as an illness in itself, rather than a symptom exhibited by many different diseases.
People did not expect healers and medicine to cure them and they certainly didn’t think that taking medicine would make them feel better. Most of the medicines that were prescribed would have made the patient feel very ill indeed. They would have been well advised to take Macbeth’s advice and “throw physic to the dogs.”
Even though it must have been evident that medicines rarely worked, they usually made the patient feel much worse, and people often died during treatment, the healer was rarely blamed for the death. Unsatisfactory results were explained away either because the malady was too severe for the treatment, or because the patient had failed to follow the often very detailed medical advice correctly. One surgeon, Tristram Lyde, ended up appearing in a Rochester court after he prescribed mercury treatments for several women suffering from syphilis who subsequently died. His defense was that the women were gravely ill and had failed to follow his instructions properly. The judge accepted the explanation and Lyde walked free.
Until germ theory was developed in the 19th century, medical practitioners were left guessing as to the cause of many diseases and therefore had little hope of treating them. Advances in medical treatment were also severely hindered by an almost complete lack of knowledge of physiology or pharmacology.
In spite of their best efforts, before the beginning of the 18th century, medical professionals had little impact on the population they treated. Death was rarely stopped or even slowed in its progress. Even identifying when death had occurred could be tricky, as we shall see.
___________________________________
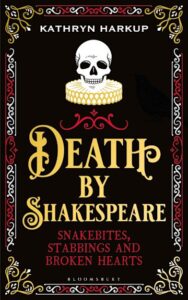
Excerpted from Death By Shakespeare: Snakebites, Stabbings and Broken Hearts by Kathryn Harkup. Copyright © 2020. Available from Bloomsbury.
Kathryn Harkup
Kathryn Harkup is a former chemist turned author. She writes and gives regular public talks on the disgusting and dangerous side of science. Her first book was the international best-seller A is for Arsenic: The Poisons of Agatha Christie, which was shortlisted for a Mystery Readers International Macavity Award and a BMA Book Award. She has also written Making the Monster: The Science of Mary Shelley’s Frankenstein, Death by Shakespeare: Snakebites, Stabbings and Broken Hearts, and her latest book, Licence to Kill: The Science of James Bond.