“Good Medicine and a Very Bad Drug...” Reckoning With the Deadly Duality of Fentanyl
Ryan Hampton Considers Addiction, Recovery, and the Human Cost of the Drug Crisis in America
The bowling ball on my chest is always heaviest at 3 a.m. Its steady pressure pushes me out of sleep most mornings before the sun rises on either coast. I could set my alarm by it, but I don’t need to. Wherever I wake up—in hotel rooms, at friends’ houses, or in the home I share with my husband—the bowling ball is there, in the pocket right between my ribs and a little bit north of my stomach.
When the weight wakes me up in the morning, it’s never for a good reason. Every day, I talk to friends, parents, loved ones, and peer workers as they face yet another unspeakable tragedy. One in ten Americans has lost someone to an overdose, and that number is only rising. An entire generation is dying off, as though killed by a plague that nobody is brave enough to name.
There are no words for these losses—these deaths. What I felt in the beginning—the hot anger and outrage that fueled my advocacy—has faded to a dull ache that sits in my body and never goes away.
It feels like grief. Or maybe, heartbreak.
[Fentanyl] was created by human beings, and we are in the middle of an all-too-human crisis.
Years after entering recovery, I need more than my fingers and toes to count the number of people I know who lost their lives to fentanyl. Within the past few years, that number has increased exponentially; it seems like fentanyl was in everything, from cocaine to fake prescription pills to bags of heroin. I left the scene at exactly the right moment—and I know that, had I continued to use, I would be dead today. Fentanyl has no discernible taste, smell, or color. The only way to tell if your substances are tainted with it is to test them—how many people living on the streets like I did, or planning to party with their friends, actually do that? I am positive that I would have been a casualty along with many of the people I cared about and used with.
There is no bad time to stop using heroin, but I am positive that I quit at exactly the right moment. In 2014, I was at the tail end of my chaotic drug use. I was more than a little worse for wear. After years of living on and off the streets, I was in bad shape. I injected black tar heroin into every vein that I could find—and they seemed to be shrinking daily, hiding under my skin while I tried to dig them out with the jagged syringe I kept on me at all times. I was the type of IV drug user you see in after-school specials—the kind they tell you to be scared of on the news. I was the addict hiding in a doorway to cook my dope in a battered spoon. I shared needles, slept where I could, and was living, one might say, just to exist.
Heroin didn’t even get me high anymore. It just made me feel like I was going to survive.
One of my last using buddies was a guy named Gor. He was close to my age, but, like me, it was hard to tell how old he was. Although he was still in his early thirties, he was battered by countless sleepless nights, never-ending withdrawal, and the anxiety of living minute to minute. His cheeks were carved hollows. His brown eyes darted from side to side. His gums bled from malnutrition, bad dope, and the endless grinding of his jaw. He was Armenian, and his curly black hair was tangled and wild. One side of his head was cropped short, where he’d cut off a matted dreadlock that bothered him. Like mine, his nails were darker and oilier than a mechanic’s. We shared the little bit we had, from spare change to the spoon we used as a cooker. We shared needles. Stories. Like me, Gor had a family—a family that loved him. Sometimes, we talked about where we came from, but often, it was just too painful.
The last time I saw Gor, we were dividing a small bag of heroin on South Hill Street in downtown Los Angeles. It was a cold Southern California night shortly after Halloween. We went through our ritual of holding the lighter under our spoon, drawing the foul-looking liquid into our syringe, and painstakingly bringing a vein to the surface of the skin. It was a pathetic amount of dope, hardly enough to take the edge off, but we still split it. Fair was fair.
“I need to get help,” I told Gor as I watched him tug his sleeve back.
“That’s great, man. You should,” he said. The needle found an open lesion on his arm and slid in. I shivered. I had never hated heroin more, or needed it more intensely.
“I’m done with this,” I told him, as I had said a hundred times, after every shot.
Little did I know that, this time, I was on my way to speaking the truth.
A few weeks after that score, I finally got into treatment—first, a detox program and then inpatient treatment that would put me on track for sober living and set me up to start getting my life back. I was grateful that I even had a bed. After years of struggling to find the help I needed, I knew how lucky I was. As it turned out, it wasn’t a moment too soon.
In my third week of treatment, my counselor finally let me check my email and Facebook under supervision. She watched me while I logged in from her computer and started scrolling through my notifications. Gor and I were Facebook friends, so I clicked on his profile.
“Gone too soon,” the posts on his wall said.
I felt the too-familiar bowling ball in my chest. How was this possible?
It was a fentanyl OD. Gor hadn’t stood a chance.
At that time, we didn’t even know fentanyl was on the streets in Los Angeles. It was a tiny ripple—a hint of the terrible tsunami that was on its way to crush us. I thought of Gor, unknowingly jabbing what would be his last load into his veins. The bag he’d bought was mixed with something else, but he had no way to tell. To him, it probably looked like our usual dose. It killed him.
That could have been me. If I’d been with Gor instead of where I was, it would have been. I felt my body turn to ice and start to shake with the realization of what I had just avoided. That bag had my number on it. I sank onto my freshly made bed and hugged myself. I’d dodged a bullet, and I could practically hear it zinging past me.
While heroin was no longer part of my life, it seemed that fentanyl was inescapable. Even in recovery, I couldn’t completely avoid it. Seven years into my recovery, I had to have an outpatient medical procedure, and the doctor told me that they’d administer fentanyl as part of my anesthesia. I panicked.
“You can’t do that,” I sputtered. “I’m in recovery! I could relapse or die.”
The doctor tried to reassure me, but I wasn’t buying it. I begged for another option, and even asked them to do the procedure without anesthesia, but there was no other way. I was terrified. I reached out to all my support people, told my friends, and hoped for the best. As I was rolled into the operating room, I said a prayer for my recovery. I didn’t want to end up like Gor. I didn’t want to go back to the misery of shooting up, chasing a high that didn’t exist for me anymore. A masked face bent over me and told me to count down from 10.
“Nine, eight,” I said. In an instant, the world went dark.
When I woke up, I was shocked by how normal I felt. The fentanyl I’d been given was a low pharmaceutical dose. It was administered by an anesthesiologist in a hospital setting where I was monitored. I expected to wake up from surgery foaming at the mouth, pulling out my IV line, and running down the street to find the nearest heroin dealer. Instead, I just felt like myself. (Well, myself plus a little bit of pain.) I’d been given the same fentanyl that is commonly used in epidurals during labor. And I was fine.
Had I been wrong about fentanyl? Was I misinformed? Yes—and no.
*
There are a lot of misconceptions swirling around fentanyl. Some law enforcement agencies believe it is a weapon of mass destruction that kills indiscriminately, like poisons or anthrax. Every September and October, like clockwork, Fox News anchors tell viewers that drug dealers are lacing Halloween candy with it. Laypeople have been told not to pick up stray dollar bills off the ground because any bill could have fentanyl on it and cause them to OD. A police department in Arkansas told shoppers to wipe down grocery carts because fentanyl residue might be on the handle. A firefighter once told me he would not give CPR to someone overdosing because he might OD if the victim’s sweat got in his mouth.
All of this is complete bullshit.
The drug has relieved pain and suffering for millions of people…but it has also caused profound pain and suffering.
People believe these sorts of myths and urban legends because they are afraid. Maybe they’ve lost friends and loved ones to addiction and overdose, and they are grieving. Maybe it’s plain old ignorance. But the truth about fentanyl is scary enough without these fantasies and fairy tales. In order to prevent more people from dying, we have to be honest about what we’re up against.
That’s why it’s critically important to reckon with the science and history of fentanyl. Fentanyl is not the boogeyman. It was created by human beings, and we are in the middle of an all-too-human crisis. It’s up to us to do something. But first, we have to see the bigger picture.
Like many other drugs today, the story of fentanyl begins with a powerful pharmaceutical company. In 1959, an ambitious chemist named Dr. Paul Janssen first synthesized the pain reliever known as fentanyl while tinkering with the chemical structure of morphine. He was only 33 and worked in a lab given to him by his father, a prominent family doctor in Belgium. In this small lab with just a few scientists, Janssen discovered a medicine that would change the world.
Unlike morphine, which is an opioid derived from the sap of poppy plants, fentanyl is completely synthetic and is made in a laboratory. That means the production of fentanyl requires no farmers, no fields of fragile flower crops, and no perfect growing climate. All it takes to create tons and tons of fentanyl is a chemist, a lab, and the right precursors (the chemicals used in the reaction that produces fentanyl).
The production of fentanyl matters a great deal when it comes to understanding how this drug came to be so widespread and available today. If you’ve seen any news stories about fentanyl, you’ve probably heard about how dangerous and potent it is. Fentanyl is at least 100 times more potent than morphine. Whereas drugs like morphine are measured in milligrams, doses of fentanyl are measured in micrograms.
Until Janssen’s creation, the world had never seen such a potent opioid. The development of synthetic opioids has marked rapid progress in the field of medicine. It revolutionized surgery. But its legacy is complicated. Like all opioids, fentanyl has a light side and a dark side. The drug has relieved pain and suffering for millions of people and has become a staple of modern medicine, but it has also caused profound pain and suffering. A lifesaving medicine in hospitals can also be a life-threatening drug on the street.
That’s why fentanyl was called a “good medicine, and a bad drug” at a recent United Nations conference. And something so powerful couldn’t be safely isolated for medical use for long. Soon, fentanyl moved out of labs and hospitals and into the hands of shady chemists and drug dealers on the streets of California.
__________________________________
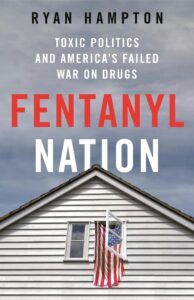
Excerpted from Fentanyl Nation: Toxic Politics and America’s Failed War on Drugs by Ryan Hampton. Copyright © 2024. Published by St. Martin’s Press, an imprint of Macmillan, Inc.
Ryan Hampton
Ryan Hampton is a national addiction recovery advocate, author, media commentator, and person in long-term recovery. He has worked with multiple non-profits nationwide to end overdose and served in leadership capacities for various community organizing initiatives. Hampton is in recovery from a decade of active opioid use and is a leading voice in America's rising recovery movement. He is the author of Unsettled and American Fix—and lives in Nevada with his husband, Sean, and their boxer dog, Quincy.