I worked as a neurosurgeon for over forty years. I lived in a world filled with fear and suffering, death and cancer. Like all doctors, I had to find a balance between compassion and detachment. This was sometimes very difficult. But rarely, if ever, did I think about what it would be like when what I witnessed at work every day happened to me. This is the story of how I became a patient.
I came to medicine by a roundabout route, which had included studying, and abandoning, philosophy. I knew only the most basic science by the time that I became a doctor. Although I am deeply fascinated by science, I am not a scientist. Most neurosurgeons are not neuroscientists—to claim that they all are would be like saying that all plumbers are metallurgists.
But as I approach the end of my life, I find myself besieged by philosophical and scientific questions that suddenly seem very important—questions which in the past I had either taken for granted or ignored. This is also the story of my attempts to understand some of these questions, without necessarily finding answers.
*
It seemed a bit of a joke at the time—that I should have my own brain scanned. I should have known better. I had always advised patients and friends to avoid having brain scans unless they had significant problems. You might not like what you see, I told them.
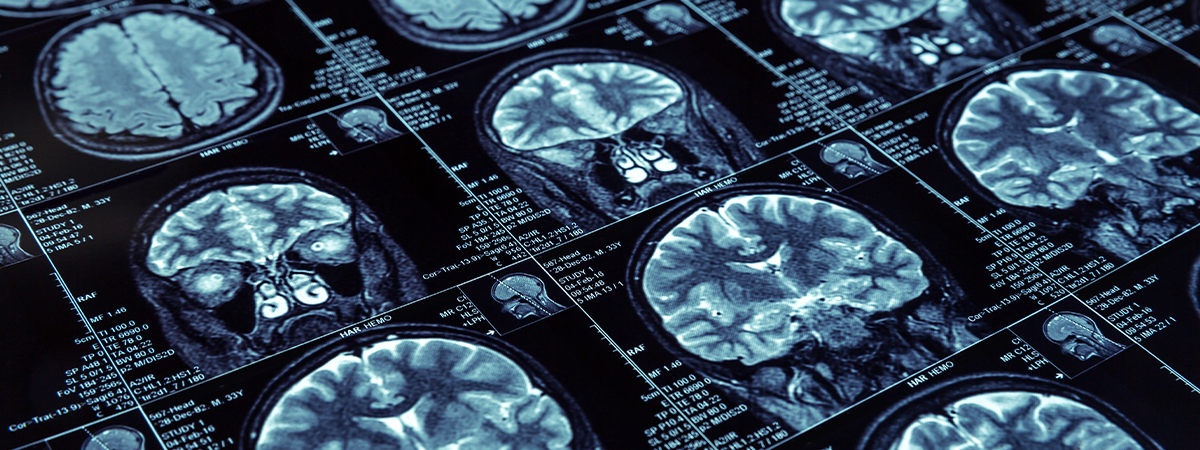
I had volunteered to take part in a study of brain scans in healthy people. I was curious to see my own brain, if only in the greyscale pixels of an MRI scan. I had spent much of my life looking at brain scans or living brains when operating, but the awe I felt as a medical student when seeing brain surgery for the first time had fallen away quite quickly once I started training as a neurosurgeon.
Besides, when you are operating you do not want to distract yourself with philosophical thoughts about the profound mystery of how the physical matter of our brains generates thought and feeling, and the puzzle of how this is both conscious and unconscious. Nor do you want to be distracted by thinking about the family of the patient under your knife, waiting, desperate with anxiety, somewhere in the world outside the theatre. You need to separate yourself from these thoughts and feelings, although they are never far away. All that matters is the operating and the self-belief it requires. You live very intensely when you operate.
When you are operating you do not want to distract yourself with philosophical thoughts about the profound mystery of how the physical matter of our brains generates thought and feeling.Perhaps I thought that seeing my own brain would confirm the fascination with neuroscience that had led me to become a neurosurgeon in the first place, and that it would fill me with a feeling of the sublime. But it was vanity. I had blithely assumed that the scan would show that I was one of the small number of older people whose brains show little sign of aging. I can now see that although I had retired, I was still thinking like a doctor—that diseases only happened to patients, and not to doctors, that I was still quite clever and had a good memory with perfect balance and coordination. I ran many miles every week and lifted weights and did manly press-ups. But when I eventually looked at my brain scan, all this effort looked like King Canute trying to stop the rising tide of the sea.
Several months passed before I could bring myself to open the CD which had been sent to me after the scan. I had found plenty of excuses to put it off—downloading the data from the CD to my computer might be complicated, I had many lecture tours abroad, things to make in my workshop, days to spend with my grandchildren. In retrospect, I can see that I was apprehensive about what the scan might show, but I had managed to repress this fear, keeping it out of conscious thought.
It took only a few minutes to download the files. As I looked at the images on my computer’s monitor, one by one, just as I used to look at my patients’ scans, slice by slice, working up from the brain stem to the cerebral hemispheres, I was overwhelmed by a feeling of complete helplessness and despair. I thought of folk stories about people who had premonitions of attending their own funeral. I was looking at aging in action, in black and white MRI pixels, death and dissolution foretold, and already partly achieved.
We accept that wrinkled skin comes with age but find it hard to accept that our inner selves, our brains, are subject to similar changes.My seventy-year-old brain was shrunken and withered, a worn and sad version of what it once must have been. There were also ominous white spots in the white matter, signs of ischaemic damage, small-vessel disease, known in the trade as white-matter hyperintensities—there are various names for them. They looked like some evil pox. Not to put too fine a point to it, my brain is starting to rot. I am starting to rot. It is the writing on the wall, a deadline.
I have always felt fear as well as awe when looking at the stars at night, although the poor eyesight that comes with age now makes them increasingly difficult to see. Their cold and perfect light, their incomprehensible number and remoteness, the near eternity of their lives are in such contrast to the brevity of mine. Looking at my brain scan brought the same feeling. The urge to avert my eyes was very great. I forced myself to work through the scan’s images, one by one, and have never looked at them again. It is just too frightening.
*
There is an extensive medical literature about the white-matter changes on my brain scan, the white matter being the billions of axons—electrical wires—that connect the grey matter, the actual nerve cells. If we reach eighty years old, most of us will have these changes. Their presence is associated with an increased risk of stroke although it is unclear whether they predict dementia or not. If we make it to eighty, we have a one in six risk of developing dementia, and the risk gets greater if we live longer.
It is true that a so-called “healthy lifestyle” reduces the risk of dementia to a certain extent (some researchers suggest 30 percent) but however carefully we live, we cannot escape the effects of aging. We can only delay them if we are lucky. Long life is not necessarily a good thing. Perhaps we should not seek it too desperately.
I have reached that age where you start to dislike seeing yourself in photographs—I look so much older than I feel myself to be, even though getting out of bed in the morning is getting more difficult each year and I become tired more quickly than in the past. My patients were no different—they would protest that they felt so young if I pointed out to them the signs of aging on their scans. We accept that wrinkled skin comes with age but find it hard to accept that our inner selves, our brains, are subject to similar changes. These changes are called degenerative in the radiological reports, although all this alarming adjective means is just age-related.
I continued to think that illness happened to patients and not to doctors, even though I was now retired.For most of us, as we age, our brains shrink steadily, and if we live long enough, they end up resembling shriveled walnuts, floating in a sea of cerebro-spinal fluid, confined within our skull. And yet we usually still feel that we are our true selves, albeit diminished, slow and forgetful. The problem is that our true self, our brain, has changed, and as we have changed with our brains, we have no way of knowing that we have changed. It is the old philosophical problem—when I wake in the morning, how can I be certain I am the same person today that I was yesterday? And as for ten years ago?
I always downplayed the extent of these age-related changes seen on brain scans when talking to my patients, just as I never spelled it out that with some operations you must remove part of the brain. We are all so suggestible that doctors must choose their words very carefully. It is so easy for doctors to forget how patients cling to every word, every nuance, of what we say to them. You can unwittingly precipitate all manner of psychosomatic symptoms and anxieties. I usually told cheerful white lies.
“Your brain looks very good for your age,” I would say, to the patients’ delight, irrespective of what the scans showed, provided that they showed only age-related changes and nothing more sinister. The patients would leave the clinic room smiling happily and feeling much better. The eminent American cardiologist Bernard Lown has written of how important it can be to lie to patients—or at least to be much more optimistic than the facts perhaps justify. He tells stories of patients of his who were close to death from heart failure but who rallied and survived when he was overly positive.
We are all so suggestible that doctors must choose their words very carefully. It is so easy for doctors to forget how patients cling to every word.Hope is one of the most precious drugs doctors have at their disposal. To tell somebody they have a 5 percent hope of surviving is almost as good as telling them they have a 95 percent chance, and a good doctor will emphasize the life-affirming 5 percent without denying or hiding the corresponding 95 per cent probability of death. It is Pandora’s Box—however many horrors and ailments come out of the box, there is always hope.
Only at the very end does hope finally flicker out. Hope is not a question of statistical probability or utility. Hope is a state of mind, and states of mind are physical states in our brains, and our brains are intimately connected to our bodies (and especially to our hearts). Indeed, the idea of a disembodied brain, promoted by the more extreme protagonists for artificial intelligence, might well be meaningless. This is not to say that being kind and hopeful will cure cancer or enable us to live for ever. The human mind is always trying to reduce all events to single causes, but most diseases are the product of many different influences, and the presence or absence of hope is only one among many.
*
I have a fine copy of an engraving by the sixteenth-century German artist Albrecht Dürer on the wall of my study, which I inherited from my mother. It shows St Jerome at his desk in his study, a beautiful medieval room with a coffered ceiling and a large window with deep reveals and small panes of crown glass, through which diagonal sunlight falls. There is a lion—the creature associated with the saint—sleeping on the floor in front of him. The story goes that he removed a thorn from its paw, and it became a sort of pet. Next to the lion is a dog, symbolizing loyalty.
St Jerome was one of the early fathers of the Christian Church. He is said to have had an enthusiastic following of wealthy widows in fifth-century Rome. One of their daughters came under his influence and his advocacy of leading an ascetic life. He was blamed for her death from what some say in retrospect sounds like anorexia nervosa. I suspect I would dislike St Jerome if I met him, and consider him to be a fanatic.
Hope is one of the most precious drugs doctors have at their disposal.And yet I love the Dürer etching, with its aura of wisdom and learning, and I once made a table modeled on the desk in the picture. There is a skull on a shelf beside St Jerome’s desk, an icon often found in images of medieval philosophers. Memento mori, a reminder of the death to come. My brain scan is no different. However hard I looked it at—and I looked very hard—it told me nothing that I did not know already: my brain is aging, my memory is not as good as it was, I move and think more slowly, I will die.
I should have known that I might not like what my brain scan showed, just as I should have known that the symptoms of prostatism that were increasingly bothering me were just as likely to be caused by cancer as by the benign prostatic enlargement that happens in most men as they age. But I continued to think that illness happened to patients and not to doctors, even though I was now retired.
Twenty months after I had my brain scanned, I was diagnosed with advanced prostate cancer. I had had typical symptoms for years, steadily getting worse, but it took me a long time before I could bring myself to ask for help. I thought I was being stoical when in reality I was being a coward. I simply couldn’t believe the diagnosis at first, so deeply ingrained was my denial.
For many years I had kept a human skull on a shelf in my study, in rather self-conscious imitation of the Dürer. I had found it discarded in a box, in a pile of rubbish, when the hospital I had worked in for many years was closed and relocated. An unknown predecessor must have been practicing on it—there was a series of burr holes in the skull’s vault, with saw cuts between them, that had clearly been made with an old-fashioned surgical hand saw that fell out of use a long time ago.
It was otherwise in unusually pristine condition, with intact stylomastoid processes, the little needles of bone behind the ear to which the stylomastoid muscles are attached. They often break off quickly with any handling of the skull. Once I had been diagnosed with advanced cancer, I no longer found the sight of the skull amusing. I gave it to one of my colleagues at the hospital where I used to work, so that he could use it for teaching.
______________________________
Henry Marsh’s And Finally is available from St. Martin’s Press